WHAT
IS THE BEST DRAINAGE METHOD FOR A PERINEPHRIC ABSCESS?
(
Download pdf )
doi: 10.1590/S1677-55382010000100005
AHMED R. EL-NAHAS, RAED FAISAL, TAREK MOHSEN, MOHAMMED S. AL-MARHOON, HASSAN ABOL-ENEIN
Department of Urology (AREN, RF, MSAM, HAE) and Radiology (TM), Urology and Nephrology Center, Mansoura University, Mansoura, Egypt
ABSTRACT
Purpose:
To compare the results of percutaneous and open drainage for perinephric
abscess.
Materials and Methods: The files of 86 patients who underwent drainage
for perinephric abscesses from April 2001 through March 2008 were evaluated.
The method of drainage for each patient was performed according to the
clinical decision of the treating physician. Percutaneous tube drain (PCD)
was used for drainage of the abscess in 43 patients (group 1), while the
other 43 patients were managed with open drainage (group 2). Cure was
defined as complete obliteration of the abscess cavity. The cure rates,
complications, and hospital stay were compared between both groups.
Results: The study included 50 males and 36 females with mean age 44.2
± 17.3. The most common predisposing factors were diabetes mellitus
and/or stones. Open drainage of perinephric abscesses resulted in a statistically
significant higher cure rate (98% versus 69%, p < 0.001) and shorter
hospital stay than PCD (3.6 versus 6 days, p < 0.001). Failure of complete
drainage of multilocular abscess was observed in 8 of 13 cases (61.5%)
in group 1 and one of 38 cases (2.6%) in group 2 (P < 0.001). Complications
were observed in 7% of group 1 and 11.5% in group 2 (P = 0.45). After
mean follow-up of 19 months, 9 of 46 patients (19.6%) had recurrence;
7 of them were in group 1.
Conclusion: Percutaneous drainage of perinephric abscess is an effective
minimally invasive treatment. However, PCD is not the optimal method for
drainage of multilocular abscess because open surgical drainage provided
higher cure rates and shorter hospitalization than PCD.
Key
words: kidney; infection; abscess; perinephric; percutaneous;
surgery
Int Braz J Urol. 2010; 36: 29-37
INTRODUCTION
Perinephric abscess (PNA) is defined as an abscess outside the renal capsule but within Gerota’s fascia. They are rare in comparison to other infections involving the genitourinary tract but they can cause significant morbidity and mortality (1). Broad-spectrum antibiotic therapy is the first step in treatment and should be associated with drainage in the majority of cases. The first report of open surgical drainage of PNA was described by the French physician Germain Colotin in 1474 (2). Surgical drainage has been the accepted practice since then. After the advent of various imaging modalities such as ultrasonography and computed tomography, percutaneous drainage (PCD) with radiological guidance has become widely used for most abdominal abscesses including selected cases of PNA (3). There have been many reported studies that have evaluated PCD as a minimally invasive treatment for PNA (3-6). Nevertheless, to our knowledge no previous series has compared PCD versus open drainage in the management of PNA. The present study was conducted to compare the efficacy and safety of open drainage with PCD in the management of PNA.
MATERIALS AND METHODS
The computerized
files, radiographic images, operative and postoperative data of 86 patients
who were treated for perinephric abscess at our center from April 2001
through March 2008 were retrospectively assessed. We included only patients
with perinephric abscess who required drainage because of either presence
of predisposing factors or large abscess size. Preoperative laboratory
workup included serum creatinine tests, complete blood count, urinalysis
and culture. Suspected patients were clinically evaluated based on detailed
medical history and physical examination results. Abdominal ultrasonography
was the initial radiological investigation. When the findings were suggestive
of perinephric abscess, unenhanced computed tomography (CT) scan of the
abdomen was performed to confirm the diagnosis and determine abscess configuration
(unilocular or multilocular), volume and associated conditions (such as
renal or ureteral stones).
All patients received a broad-spectrum of intravenous antibiotics (third
generation cephalosporin), then PCD or open drainage was considered. The
method of drainage for each patient was performed according to the clinical
decision of the treating physician. PCD was chosen for severely ill patients
who could not withstand general anesthesia. It was performed by a radiologist
under local anesthesia using ultrasound guidance. A pigtail catheter of
12 or 14F was percutaneously inserted into the abscess cavity. Open drainage
was performed under general anesthesia through a small flank incision.
When the abscess cavity was entered, a gentle opening of all locules was
performed. This was followed by irrigation of the abscess cavity with
saline and gentamycin. Two wide caliber tube drains (24F) were left indwelling.
Drainage catheters remained in place until the output was minimal and
radiographic resolution was confirmed with ultrasonography. Cure was defined
as complete obliteration of the abscess cavity. The patients were discharged
from the hospital when they were clinically improved and free of any tubes.
Patients were evaluated during follow-up visits for abscess recurrence
by ultrasonography.
Percutaneous tube drain was inserted for drainage of the abscess in 43
patients (Group 1), while the other 43 patients were managed with open
surgical drainage (Group 2). In 20 patients with hydronephrosis due to
obstructing stones, urinary drainage with percutaneous nephrostomy tube
(6) or double J stent (14) was also performed.
The cure rate, complications, hospital stay and recurrence were compared
in both groups using chi-square and Student’s-t-test or Mann-Whitney
test.
RESULTS
The study included 50 males and 36 females with a mean age of 44.2 ± 17.3. Demographic data, predisposing factors and presentations are summarized in Table-1. The most common predisposing factors were diabetes mellitus and/or kidney stones. In 11 patients, the condition was associated with distant skin or subcutaneous abscess. It was observed that the success rate was 77% in diabetic patients compared with 88% in non-diabetic patients, but the difference was not statistically significant (p = 0.184).
Preoperative laboratory and radiological
data are summarized in Table-2.
The differences between cure rates, complications
and hospital stay of group 1 and 2 are presented in Table-3. There was
no significant difference between the complication rates of both groups.
In group 1, recurrent post-drainage fever was encountered in 2 patients
and was controlled by intravenous antibiotics and antipyretics. In group
2, two cases of wound infection were managed by frequent dressing changes
and a case of wound dehiscence required secondary sutures. Intra-operative
bleeding from inadvertent inferior vena cava injury was adequately repaired
with 4/0 sutures and blood transfusion. Septic shock developed in one
patient in each group and admission to the intensive care unit was necessary.
One of them was resuscitated with cardiac inotropic drugs, intravenous
fluids and antibiotics, while the other died from septic shock.
Open drainage of perinephric abscesses resulted
in statistically significant higher cure rate and shorter hospital stay
than PCD (p < 0.001). Inadequate drainage was found in 17 cases of
group 1; 7 of them were managed by readjustment of the PCD (replacement
of the PCD with wider tube in the same locule or insertion of another
PCD in other locules of the abscess) while the remaining 10 cases needed
further open drainage. Inadequate drainage was observed in only one patient
of group 2. This was due to missing one locule of a multilocular abscess
and it was managed with PCD. The abscess configuration had a significant
effect on the outcome. Failure of complete drainage of multilocular abscess
was found in 8 of 13 cases (61.5%) in group 1 and one of 38 cases (2.6%)
in group 2 (P < 0.001). On the other hand, incomplete drainage of a
unilocular abscess was observed in one of 29 cases (82%) in group 1 (because
of large abscess volume with thick pus) and none of 5 cases (100%) in
group 2 (p = 0.315).
Eight patients required delayed nephrectomy
for non-functioning ipsilateral kidney. After mean follow-up of 16.7 months
(range 3-65), 9 out of 46 patients (19.6%) suffered recurrence of PNA
in the ipsilateral side, 7 of them were in group 1.
COMMENTS
While
urinary tract infections are common, the severe complications of renal
and perinephric abscess formation are uncommon and usually occur in patients
with predisposing factors such as diabetes mellitus, urinary calculi,
urinary obstruction and immune compromised patients. Moreover, multiple
predisposing factors may be present in the same patient (1). The same
findings were observed in the present study. We identified diabetes, urolithiasis,
and immune-compromised conditions as predisposing factors for PNA and
in some patients multiple factors were present (Table-1).
Prior to the development and availability
of antibiotics, most perinephric abscesses were due to hematogenous spread
of gram positive bacterial infection (such as Staphylococcus aureus) resulting
in formation of renal cortical abscess (7,8). Currently, the majority
of perinephric abscesses are due to gram negative bacteria which ascend
in a retrograde fashion from the lower urinary tract causing corticomedullary
abscess (9). A PNA is formed when a cortical or corticomedullary abscess
eventually rupture into the perinephric space. Opportunistic organisms
such as Candida albicans are also isolated from immune suppressed and
diabetic patients (10). In the present study, the most common isolated
organisms were gram negative bacilli (such as Escherichia coli and Klebsiella
pneumonia), while Staphylococcus aureus was isolated from 13% of patients.
Traditionally, PNA has been associated with
significant morbidity and high rates of mortality reaching up to 56% (11).
This was attributed to delay in diagnosis because the symptoms of PNA
are somewhat non-specific and confusing. Due to the introduction of cross-sectional
imaging modalities such as CT, in addition to improvement of ultrasound
examinations, early diagnosis and minimally invasive treatment represent
major advances in management of PNA during the last 20 years.
The wide spread utilization of ultrasound
for examination of patients with loin pain, fever or other non-specific
complaints has resulted in early diagnosis of PNA. When there is any suspicion
regarding the nature of the lesion, CT is a valuable tool for confirmation
of the diagnosis (11). Therefore, the mortality rates in recent series
have decreased to 12%-14% (1,12). The authors attributed mortality among
their patients to medical treatment of abscesses that otherwise needed
drainage. In the present study, we used ultrasound for evaluation of all
patients with suspicious symptoms or predisposing factors of PNA and CT
was used in to confirm the diagnosis. Then, we drained PNA that were large
or present in patients with predisposing factors. This may be the reason
for very low mortality rate (1%) among our patients.
The classic open surgical drainage for perinephric
abscess has been challenged by the introduction of image guided percutaneous
tube drainage methods and antibiotics alone (12). The general consensus
is that large abscesses and patients with predisposing factors require
drainage in addition to antibiotics (12,13). Therefore, antibiotics without
drainage are suitable for selected cases and the decision to treat with
antibiotics alone requires consideration of other associated medical conditions
(1). The reason for not using antibiotics alone in our patients was either
presence of predisposing factors or large abscess size.
Percutaneous drainage with radiological
guidance has become the treatment of choice for most abdominal abscesses
as it usually provides satisfactory clinical results with minimal complications,
thus obviates the need for open surgery (14). Percutaneous drainage of
PNA has been reported in many series (3-6). The ease of image guided fixation
of PCD without the need for general anesthesia has made it the preferred
choice for severely ill patients. Moreover, the cure rate of 60-67% was
the main reason that made PCD the most commonly used minimally invasive
intervention for treatment of PNA. The main disadvantage was the need
for adjustment or insertion of multiple draining tubes in many patients
(1,3-6,13). In the present study, PCD was able to adequately drain the
abscess in 60% of patients, and subsequently the cure rate was increased
to 69%, after adjustment of the tube in 7 patients. Another disadvantage
of PCD was the longer hospital stay because of slow drainage or the need
for multiple interventions.
In our study, the main cause of PCD failure
was multilocular abscess cavity. The PCD can only drain the locule at
its site of insertion. Therefore, it may be beneficial to fix multiple
tubes from the start in multilocular abscess. On the other hand, a quick
extraperitoneal open drainage provided very high cure rate (98%) even
in patients with multilocular abscess because of manually disrupting the
septa between the abscess locules. Moreover, evacuation of thick pus during
open drainage and wide draining tubes resulted in significantly shorter
hospital stay. However, these achievements were gained at the expense
of using a general anesthesia and a slightly higher complication rate
than PCD. It is also important to emphasis that severely ill patients
cannot tolerate nephrectomy of a non-functioning kidney at the time of
PNA drainage. Therefore, delayed nephrectomy was performed in 8 patients
following complete abscess drainage and improvement of the patients’
general condition.
Although the selection bias for each treatment
option cannot be completely eliminated, it was statistically proven in
our study that PCD was not the optimal drainage method for multilocular
PNA. This was based on the lower cure rate of PCD in the treatment of
multilocular PNA and the higher recurrence rate that may have resulted
from enlargement of a very small residual. However, a prospective randomized
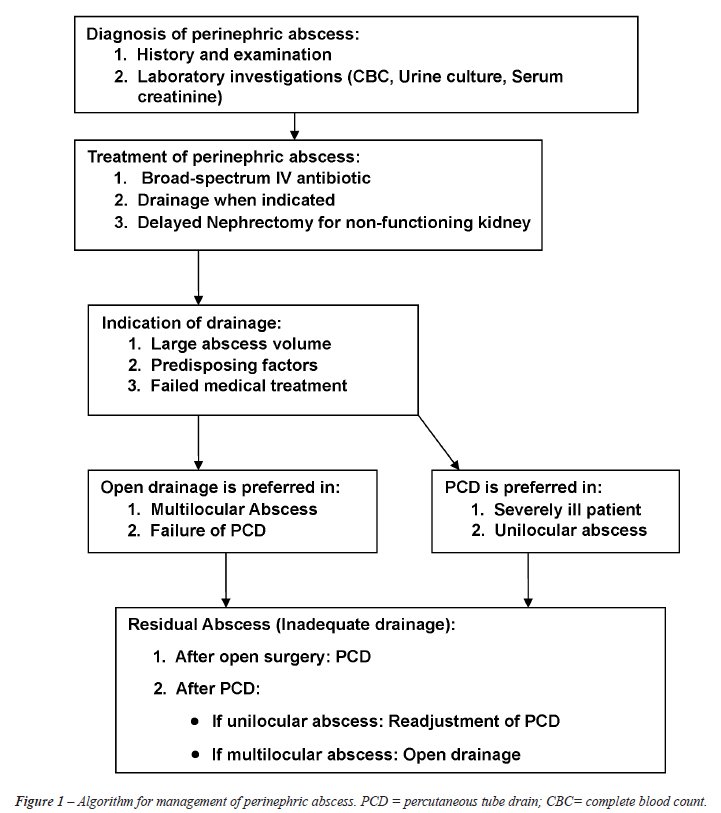
trial is warranted to confirm these findings. A proposed algorithm for
treatment of perinephric abscess is illustrated in Figure-1.
CONCLUSIONS
Percutaneous drainage of a perinephric abscess is an effective minimally invasive treatment modality. Therefore, when a PNA has to be drained, we recommend PCD as the primary drainage method because, as shown in our series, it can save 69% of patients an open surgery. However, and after acknowledging the limitations of the retrospective nature of the study. PCD is not the optimal method for drainage of multilocular abscess because open surgical drainage provided higher cure rates, shorter hospitalization and lower recurrence rate than PCD.
ACKNOWLEDGMENT
Dr. Mohamed Motwally assisted in data collection.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Meng MV, Mario LA, McAninch JW: Current treatment and outcomes of perinephric abscesses. J Urol. 2002; 168: 1337-40.
- Morgan WR, Nyberg LM Jr: Perinephric and intrarenal abscesses. Urology. 1985; 26: 529-36.
- Siegel JF, Smith A, Moldwin R: Minimally invasive treatment of renal abscess. J Urol. 1996; 155: 52-5.
- Gerzof SG, Gale ME: Computed tomography and ultrasonography for diagnosis and treatment of renal and retroperitoneal abscesses. Urol Clin North Am. 1982; 9: 185-93.
- Deyoe LA, Cronan JJ, Lambiase RE, Dorfman GS: Percutaneous drainage of renal and perirenal abscesses: results in 30 patients. AJR Am J Roentgenol. 1990; 155: 81-3.
- Lang EK: Renal, perirenal, and pararenal abscesses: percutaneous drainage. Radiology. 1990; 174: 109-13.
- Truesdale BH, Rous SN, Nelson RP: Perinephric abscess: a review of 26 cases. J Urol. 1977; 118: 910-1.
- Jemni L, Mdimagh L, Jemni-Gharbi H, Jemni M, Kraiem C, Allegue M: Kidney carbuncle: diagnostic, bacteriological and therapeutic considerations. Apropos of 11 cases. J Urol (Paris). 1992; 98: 228-31.
- Noble MJ: Perinephric abscess. AUA update. Series 2002; Vol. XXI, Lesson 10; 74-79.
- Patterson JE, Andriole VT: Bacterial urinary tract infections in diabetes. Infect Dis Clin North Am. 1997; 11: 735-50.
- Salvatierra O Jr, Bucklew WB, Morrow JW: Perinephric abscess: a report of 71 cases. J Urol. 1967; 98: 296-302.
- Rai RS, Karan SC, Kayastha A: Renal and perinephric abscesses revisited. MJAFI 2007; 63: 223-225.
- Coelho RF, Schneider-Monteiro ED, Mesquita JL, Mazzucchi E, Marmo Lucon A, Srougi M: Renal and perinephric abscesses: analysis of 65 consecutive cases. World J Surg. 2007; 31: 431-6.
- vanSonnenberg E, Mueller PR, Ferrucci JT Jr: Percutaneous drainage of 250 abdominal abscesses and fluid collections. Part I: Results, failures, and complications. Radiology. 1984; 151: 337-41.
____________________
Accepted after revision:
September 18, 2009
_______________________
Correspondence address:
Dr. Ahmed R. El-Nahas
Urology & Nephrology Center
Mansoura University
Mansoura, Egypt
Fax: + 2050 2263717
E-mail: ar_el_nahas@yahoo.com
EDITORIAL COMMENT
Perinephric abscess is a serious entity neglected in the urological literature.
Morbidity and mortality have fallen in the last decades thanks to the
progress in diagnosis with ultrasonography and overall computed tomography
(CT) scan and due to improvement in medical and surgical therapies. Nevertheless,
the best way of surgical management of such collections has been a subject
of debate. In this article, the authors compared retrospectively the outcome
of 43 perinephric abscess drained percutaneously with 43 cases drained
by open surgery. Renal stones and diabetes mellitus were the most important
predisposing factors. Abscesses drained by open surgery were significantly
greater and multiloculated when compared to percutaneously drained abscesses.
The cure rate was significantly higher in the group treated by the open
access. There were no difference in the complication rate but hospital
stay was longer among patients treated percutaneously.
This article concerns three important issues: A) Perinephric abscesses
occur with some frequency and must be always suspected in patients with
prolonged fever, overall in diabetics and in patients with stones, B)
CT is an important tool and should be considered the gold-standard, not
only in early diagnosis but also in the planning of the therapy to be
instituted, and C) Minimally invasive therapy is not always the best option.
In fact, as the authors clearly showed, a quick open drainage is more
efficient especially in multiloculated collections. In this setting percutaneous
drainage should be reserved for patients in a severe clinical condition,
when it can be performed under local anesthesia or for uniloculated abscesses
with greater chance of success.
The results corroborate those obtained by Coelho et al. (1) that also
found diabetes mellitus and stones as the main predisposing factors for
perinephric abscesses and by Meng et al. (2) who showed that CT could
influence prognosis as it allows for earlier diagnosis and that a 36%
failure rate with percutaneous drainage can be observed in such cases.
Another important point is that small perinephric collections (usually
less than 2 cm) can be managed successfully with adequate antibiotics
and correction of eventual predisposing factors like urinary obstruction
(2).
REFERENCES
- Coelho RF, Schneider-Monteiro ED, Mesquita JL, Mazzucchi E, Marmo Lucon A, Srougi M: Renal and perinephric abscesses: analysis of 65 consecutive cases. World J Surg. 2007; 31: 431-6.
- Meng MV, Mario LA, McAninch JW: Current treatment and outcomes of perinephric abscesses. J Urol. 2002; 168: 1337-40.
Dr.
Eduardo Mazzucchi
Division of Urology
Medical School, University of Sao Paulo, USP
Sao Paulo, SP, Brazil
E-mail: mazuchi@terra.com.br
EDITORIAL COMMENT
This paper
compared 2 methods of drainage for perinephric abscess: percutaneous versus
open surgical drainage. The authors found that open drainage was associated
with higher cure rates, lower recurrence rates and shorter hospital stay,
particularly in patients with multilocular abscess. They correctly emphasized
that percutaneous drainage is the first line option of treatment in severely
ill patients with perinephric unilocular abscess. Currently, perinephric
abscesses are uncommon in most urology units (1) and since 1998, in my
unit, we have seen fewer cases. It is therefore refreshing to read about
the experience of a unit where this clinical entity remains a common clinical
problem.
A major flaw of this paper is that it was a retrospective analysis and
the patients had many variables as shown in tables 1 and 2. For example,
the authors stated that percutaneous drainage was chosen for severely
ill patients who could not withstand general anesthesia. The longer hospital
stay and higher recurrence rates in patients subjected to percutaneous
drainage could be attributed to the fact that they presented with worse
initial disease, compared to those who underwent open drainage. The location
of the abscesses, their configuration, etc., are variables that may affect
the success of percutaneous drainage. However, the paper contains some
useful guidelines (Figure-1) for units that do not have adequate experience
in the management of these patients. It must be stated that a randomized
controlled study will be difficult to carry out in patients with perinephric
abscess because of its declining incidence, the variable ways in which
patients can present and many other variables in individual patients with
the disease. A last point that is worth emphasizing is that, as in patients
with emphysematous pyelonephritis, a differential renogram test should
be carried out as soon as possible in patients with moderate to severe
perinephric abscess (1). Patients found to have poorly functioning kidneys
(< 15%) or non-functioning kidneys are best served by nephrectomy as
soon as possible rather than open or prolonged percutaneous drainage.
Nephrectomy has been shown to reduce morbidity and mortality in patients
with perinephric abscess (1).
REFERENCE
- Abdul-Halim H, Kehinde EO, Abdeen S, Lashin I, Al-Hunayan AA, Al-Awadi KA: Severe emphysematous pyelonephritis in diabetic patients: diagnosis and aspects of surgical management. Urol Int. 2005; 75: 123-8.
Dr.
Elijah O. Kehinde
Professor of Urological Surgery
Division of Urology, Department of Surgery
Faculty of Medicine, Kuwait University
Safat, Kuwait
E-mail: ekehinde@hsc.edu.kw
REPLY BY THE AUTHORS
We agree with all the comments of Dr. Eduardo Mazzucchi. Concerning the comments of Dr. Elijah O. Kehinde, we have to emphasis some points. First, the reference he mentioned is dealing with emphysematous pyelonephritis not perinephric abscess (PNA). Second, we recommended percutaneous drainage (PD) for PNA in patients with severe illness and also for patients with unilocular abscess cavity (as mentioned in figure 1 and in the discussion and conclusion). Lastly, we disagree with the comment that “non-functioning kidneys are best served by nephrectomy as soon as possible rather than open or prolonged percutaneous drainage.” This can be true for nephrectomy in case of emphysematous pyelonephritis because it is a chronic inflammation, but PNA is an acute inflammatory condition. We still advise drainage of the abscess with either PCD or open surgery. Then nephrectomy for poorly functioning kidney can be delayed until improvement of the patient’s general condition and recovery from the toxemia of an acute abscess.
The
Authors