RISK
OF CATECHOLAMINE CRISIS IN PATIENTS UNDERGOING RESECTION OF UNSUSPECTED
PHEOCHROMOCYTOMA
(
Download pdf )
Clinical Urology
Vol. 37 (1):
35-41, January - February, 2011
doi: 10.1590/S1677-55382011000100005
GINA SONG, BONNIE N. JOE, BENJAMIN M. YEH, MAXWELL V. MENG, ANTONIO C. WESTPHALEN, FERGUS V. COAKLEY
Departments of Radiology (GS, BNJ, BMY, ACW, FVC) and Urology (MVM), University of California San Francisco, San Francisco, California, USA
ABSTRACT
Purpose:
To report the risk of catecholamine crisis in patients undergoing resection
of unsuspected pheochromocytoma.
Materials and Methods: Over a four-year
period, we retrospectively identified four patients who underwent resection
of adrenal pheochromocytoma in whom the diagnosis was unsuspected based
on preoperative clinical, biochemical, and imaging evaluation.
Results: None of the patients exhibited
preoperative clinical features of catecholamine excess. Preoperative biochemical
screening in two patients was normal. CT scan performed in all patients
demonstrated a nonspecific enhancing adrenal mass. During surgical resection
of the adrenal mass, hemodynamic instability was observed in two of four
patients, and one of these two patients also suffered a myocardial infarct.
Conclusion: Both surgeons and radiologists
should maintain a high index of suspicion for pheochromocytoma, as the
tumor can be asymptomatic, biochemically negative, and have nonspecific
imaging features. Resection of such unsuspected pheochromocytomas carries
a substantial risk of intraoperative hemodynamic instability.
Key
words: adrenal gland neoplasms; imaging; surgery; pheochromocytoma;
catecholamines
Int Braz J Urol. 2011; 37: 35-41
INTRODUCTION
While there is widespread awareness of the classical clinical and radiological features of pheochromocytoma, it is perhaps less well known that 10% of pheochromocytomas are not associated with symptoms of excess catecholamine production, and up to 35% of pheochromocytomas have atypical imaging findings (1-5). Accordingly, the diagnosis may be unsuspected, and an indeterminate adrenal or retroperitoneal mass that is actually a pheochromocytoma could undergo resection without preoperative commencement of biochemical blockade. Such a patient is then at risk for a potentially a life-threatening intraoperative catecholamine crisis. However, while the risks of iodinated contrast administration and percutaneous biopsy have been reported in these unsuspected pheochromocytomas (6-8), to our knowledge, the risk of surgery in this population has not been well described. We recently encountered several patients who underwent surgical resection of unsuspected pheochromocytomas. Therefore, we undertook this study to report the risk of catecholamine crisis in patients undergoing resection of unsuspected pheochromocytoma.
MATERIALS AND METHODS
This was a retrospective study approved by our Committee on Human Research with waiver of the requirement for informed consent. Four cases of pathologically proven pheochromocytoma that underwent attempted surgical resection were identified by the study authors between 2004 and 2007. All available imaging studies and medical records of these patients were reviewed by the principal investigator. Preoperative imaging consisted of CT scan examination obtained with multiple contiguous axial images performed in the venous phase following intravenous contrast agent in all four patients with additional delayed phases obtained in two patients. One of the patients also underwent whole body PET scan after the administration of 16.4 milliCurie intravenous fluoro-2-deoxy-D-glucose (FDG) and utilizing attenuation-corrected regional emission images. None of the patients underwent imaging with iodine-131-meta-iodobenzylguanidine. The diagnosis of pheochromocytoma was confirmed by pathology of the surgically resected specimen in all four patients.
RESULTS
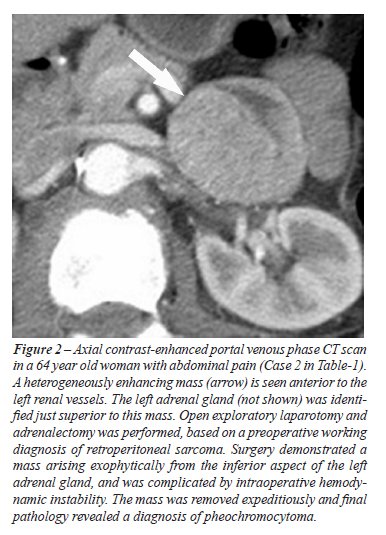
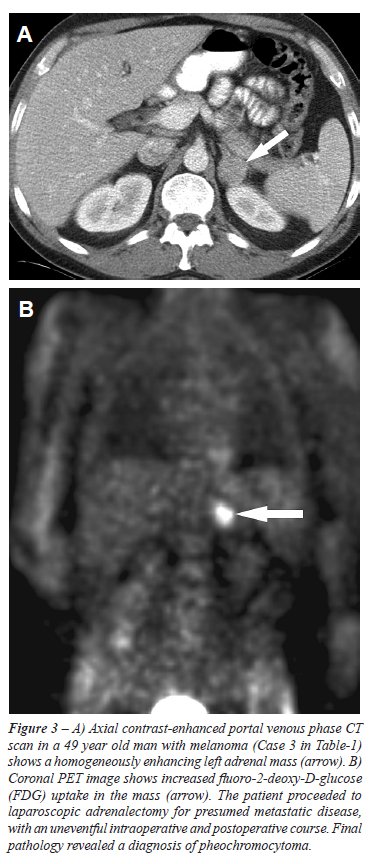
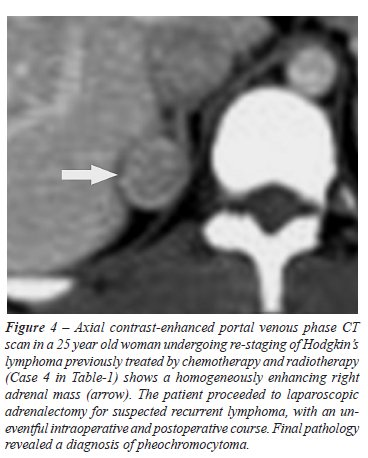
The
clinical and radiologic characteristics and intraoperative and postoperative
course of the four patients in this study are summarized in Table-1. Three
of the patients underwent imaging for purposes of staging a malignancy,
and one patient underwent imaging for abdominal pain. None of the four
patients exhibited preoperative clinical features of catecholamine excess.
One patient underwent serologic analysis, which demonstrated normal levels
of plasma metanephrine and normetanephrine. Another patient underwent
urinary analysis, which demonstrated normal levels of urinary vanillyl-mandelic
acid and normetanephrine. All patients demonstrated an adrenal mass (mean
diameter 2.7 cm, range 1.7 to 4.5 cm) with associated heterogeneous (n
= 2) or homogeneous (n = 2) enhancement on CT scan. Delayed images obtained
in two cases demonstrated less than fifty percent washout. One patient
had additional imaging with PET, which demonstrated increased FDG uptake
within the lesion. The radiological findings of the four patients are
highlighted in Figures-1 to 4. All 4 patients proceeded to adrenalectomy,
either open (n = 2) or laparoscopic (n = 2). The intraoperative course
of two patients was notable for blood pressure lability peaking at 200/100
to 220/110 mmHg systolic/diastolic. The postoperative course of one of
these two patients was complicated by an elevated troponin level to 9.7
and an electrocardiogram consistent with a non Q-wave myocardial infarction.

COMMENTS
Our
study illustrates the importance of keeping a high index of suspicion
for the possibility of pheochromocytoma for any retroperitoneal mass.
While hemodynamic instability associated with surgical and laparoscopic
resection of known or suspected pheochromocytoma has been reported (9,10),
the risk of resection in the population of unsuspected pheochromocytoma
has not been well described to our knowledge. Two out of four of our patients
demonstrated intraoperative hemodynamic instability that may have been
prevented by appropriate preoperative alpha-blockade. The postoperative
morbidity in our population might also have been averted, as the myocardial
infarction of one of our patients was presumably related to the sudden
intraoperative hypertensive challenge.
Defining typical characteristics of a pheochromocytoma
by CT is difficult as heterogeneous enhancement and poor washout as well
as FDG uptake on PET may also be seen in a metastasis or adenoma (1,4,11).
Further imaging by magnetic resonance (MR) is also problematic, as up
to 35% of pheochromocytomas do not exhibit the “lightbulb bright”
high T2 signal classically associated with pheochromocytomas (1). Current
guidelines on preoperative diagnosis thus include additional studies after
diagnosis of an adrenal mass with nonspecific characteristics on cross-sectional
imaging. Metaiodobenzylguanidine (MIBG) reportedly has an excellent specificity
of up to 100% and may increase the sensitivity of pheochromocytoma detection
to around 80% (10,12). Given the suboptimal sensitivity of biochemical
markers alone, a combination of MIBG imaging supplemented with biochemical
testing is currently recommended (12,13). Such an imaging approach may
result in better preoperative identification of pheochromocytomas, and
facilitate commencement of pre-operative alpha blockade. Both appropriate
pretreatment with alpha blockade and readily available intraoperative
antihypertensive agents have been shown to decrease intraoperative lability
(14). While pretreatment does not exclude the possibility of intraoperative
fluctuations in blood pressure (9,10), more favorable blood pressure control
may be achieved with a combination of pretreatment and intraoperative
medications (15). In a recent series of 24 patients who underwent laparoscopic
adrenalectomy for adrenal pheochromocytoma (most were treated pre-operatively
with prazosin), no cases of intra-operative hemodynamic instability were
reported (16). While such pharmacological blockade may prevent clinically
significant hemodynamic changes, it may not prevent biochemical changes.
For example, analysis of serial catecholamine levels in 11 patients undergoing
12 laparoscopic adrenalectomies while being maintained on an intravenous
alpha 1 blocker showed significant elevations related to the induction
of pneumoperitoneum and manipulation of the adrenal gland (17).
Our report has several limitations. The
study is a small retrospective case series, and cases were not identified
systematically. Patients with enhancing adrenal masses with poor washout
or increased FDG uptake at PET imaging undergoing resection were not studied
prospectively, and as such, the frequency of pheochromocytoma in adrenal
masses with nonspecific imaging characteristics is unknown. Only two out
of four patients received screening for catecholamines, and systematic
evaluation of the rate of false negatives either by urinary or plasma
analysis was therefore not made. Further imaging with MIBG was not obtained
in any of our patients, and the rate of false negatives by MIBG was thus
not obtained.
In conclusion, we report that two of four
patients who underwent resection of unsuspected pheochromocytoma sustained
intraoperative hemodynamic instability. This study emphasizes the asymptomatic
presentation, nonspecific imaging characteristics, potential for false
negative preoperative laboratory analysis, and resultant risk of catecholamine
crisis in patients with adrenal masses. Accordingly, both surgeons and
radiologists should maintain a high index of suspicion for pheochromocytoma
before resection of nonspecific adrenal masses even in asymptomatic patients.
Further studies to better delineate the imaging and biochemical preoperative
evaluation of these patients are required.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Blake MA, Kalra MK, Maher MM, Sahani DV, Sweeney AT, Mueller PR, et al.: Pheochromocytoma: an imaging chameleon. Radiographics. 2004; 24 (Suppl 1): S87-99.
- Mayo-Smith WW, Boland GW, Noto RB, Lee MJ: State-of-the-art adrenal imaging. Radiographics. 2001; 21: 995-1012.
- Sutton MG, Sheps SG, Lie JT: Prevalence of clinically unsuspected pheochromocytoma. Review of a 50-year autopsy series. Mayo Clin Proc. 1981; 56: 354-60.
- Dunnick NR, Korobkin M: Imaging of adrenal incidentalomas: current status. AJR Am J Roentgenol. 2002; 179: 559-68.
- Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR: The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev. 2004; 25: 309-40.
- Mukherjee JJ, Peppercorn PD, Reznek RH, Patel V, Kaltsas G, Besser M, et al.: Pheochromocytoma: effect of nonionic contrast medium in CT on circulating catecholamine levels. Radiology. 1997; 202: 227-31.
- Bessell-Browne R, O’Malley ME: CT of pheochromocytoma and paraganglioma: risk of adverse events with i.v. administration of nonionic contrast material. AJR Am J Roentgenol. 2007; 188: 970-4.
- Casola G, Nicolet V, vanSonnenberg E, Withers C, Bretagnolle M, Saba RM, et al.: Unsuspected pheochromocytoma: risk of blood-pressure alterations during percutaneous adrenal biopsy. Radiology. 1986; 159: 733-5.
- Kinney MA, Warner ME, vanHeerden JA, Horlocker TT, Young WF Jr, Schroeder DR, et al.: Perianesthetic risks and outcomes of pheochromocytoma and paraganglioma resection. Anesth Analg. 2000; 91: 1118-23.
- Bravo EL, Tagle R: Pheochromocytoma: state-of-the-art and future prospects. Endocr Rev. 2003; 24: 539-53.
- Yoon JK, Remer EM, Herts BR: Incidental pheochromocytoma mimicking adrenal adenoma because of rapid contrast enhancement loss. AJR Am J Roentgenol. 2006; 187: 1309-11.
- Guller U, Turek J, Eubanks S, Delong ER, Oertli D, Feldman JM: Detecting pheochromocytoma: defining the most sensitive test. Ann Surg. 2006; 243: 102-7.
- Kudva YC, Sawka AM, Young WF Jr: Clinical review 164: The laboratory diagnosis of adrenal pheochromocytoma: the Mayo Clinic experience. J Clin Endocrinol Metab. 2003; 88: 4533-9.
- Weismann D, Fassnacht M, Schubert B, Bonfig R, Tschammler A, Timm S, et al.: A dangerous liaison--pheochromocytoma in patients with malignant disease. Ann Surg Oncol. 2006; 13: 1696-701.
- Chung PC, Ng YT, Hsieh JR, Yang MW, Li AH: Labetalol pretreatment reduces blood pressure instability during surgical resection of pheochromocytoma. J Formos Med Assoc. 2006; 105: 189-93.
- Castilho LN, Simoes FA, Santos AM, Rodrigues TM, dos Santos Junior CA: Pheochromocytoma: a long-term follow-up of 24 patients undergoing laparoscopic adrenalectomy. Int Braz J Urol. 2009; 35: 24-31; discussion 32-5.
- Rocha MF, Tauzin-Fin P, Vasconcelos PL, Ballanger P: Assessment of serum catecholamine concentrations in patients with pheochromocytoma undergoing videolaparoscopic adrenalectomy. Int Braz J Urol. 2005; 31: 299-307; discussion 307-8.
____________________
Accepted after revision:
August 3, 2010
_______________________
Correspondence address:
Dr. Fergus Coakley
Chief, Abdominal Imaging
University of California San Francisco
Box 0628, M-372, 505 Parnassus Avenue
San Francisco, CA 94143-0628, USA
E-mail: fergus.coakley@radiology.ucsf.edu
EDITORIAL COMMENT
The
authors of this paper deserve to be complimented because, despite the
modest data, that was analyzed retrospectively, they raise some issues
that are very relevant for those who study and treat adrenal diseases.
First of all, they point out that adrenal
masses, and I would add retroperitoneal masses in general, can be pheochromocytomas
or paragangliomas without clinical signs or with very subtle symptoms,
which do not lead the physician to consider lesions that produce adrenergic
substances. In my personal experience (1-3), I had the opportunity to
find some pheochromocytomas that had not been diagnosed preoperatively,
much like the authors of this paper. Even worse, I found pheochromocytomas
that had been diagnosed by endocrinologists as non-functioning, which
produced adrenergic discharges in the operating room, causing all of the
risks described by the authors.
Secondly, the authors show that any surgeon is likely to encounter a patient
that has not been properly diagnosed and reacts to what he believes to
be a pheochromocytoma in the beginning of the procedure, causing hemodynamic
instability. This creates a dilemma to the surgical team: move forward
or abort the procedure? In my personal opinion, the safest measure is
to stop the procedure and adequately prepare the patient for another surgery
30 or 45 days later. However, I acknowledge that if the team is very experienced
(both surgeons and anesthesiologists), in a hospital with all the necessary
resources (medications and support), the procedure can be carried out
with good chances of success.
Finally, and this is the main point of my
analysis before the facts that were presented by the authors, each case
of adrenal mass or retroperitoneal mass suspected of being a pheochromocytoma
or a paraganglioma, regardless of the existence of symptoms, must be exhaustively
analyzed by an endocrinologist with expertise in adrenal diseases. Personally,
I do not consider myself capable of making such evaluation and I believe
that most adrenal surgeons are not. From my own personal experience, I
believe that most endocrinologists are not capable of performing this
task.
REFERENCES
- Castilho LN: Laparoscopic adrenalectomy--experience of 10 years. Arq Bras Endocrinol Metabol. 2004; 48: 776-83.
- Castilho LN, Simoes FA, Santos AM, Rodrigues TM, dos Santos Junior CA: Pheochromocytoma: a long-term follow-up of 24 patients undergoing laparoscopic adrenalectomy. Int Braz J Urol. 2009; 35: 24-31; discussion 32-5.
- Castilho LN, Castillo OA, Dénes FT, Mitre AI, Arap S: Laparoscopic adrenal surgery in children. J Urol. 2002; 168: 221-4.
Dr.
Lísias Nogueira Castilho
Section of Urology
Catholic University Campinas
Campinas, SP, Brazil
E-mail: lisias@dglnet.com.br