ENDOPYELOTOMY
WITH THE ACUCISE™ CATHETER
(
Download pdf )
ARTUR H. BRITO, ANUAR I. MITRE, SAMI ARAP
Division of Urology, School of Medicine, University of São Paulo (USP), São Paulo, SP, Brazil
ABSTRACT
Objectives:
Determine the efficiency of the Acucise™ catheter in the treatment
of ureteropelvic junction (UPJ) obstruction.
Materials and Methods: Between May 1997
and April 1999, 30 patients with primary or secondary ureteropelvic junction
obstruction were treated using Acucise™ endopyelotomy catheter. The
diagnosis was based on intravenous urography and diuretic renography.
None of the patients underwent imaging studies for identification of blood
vessels at the UPJ region. Twenty-one patients presented mild pyelocalyceal
dilation and 9 had severe pyelocalyceal dilation. As for etiology, primary
stricture was found in 24 patients and secondary stricture in 6. Three
patients had UPJ obstruction associated with homolateral renal lithiasis.
Retrograde Acucise™ endopyelotomy was performed in 27 patients; the
antegrade access was used in 3 patients that had associated renal calculi.
Incision of the stricture was performed laterally in all patients under
fluoroscopic guidance. A 7F double-J catheter was placed immediately following
the procedure, and removed after 6 weeks. Antegrade pyelotomy required
a hospital stay of 3 days and retrograde pyelotomy required 1 day.
Results: Postoperative intravenous urography
and diuretic renography demonstrated good results in 26 patients (86.6%).
Conclusions: Acucise™ endopyelotomy
represents a minimally invasive therapeutic option and can be used both
in adults and in children 8 years old and above. Patients with UPJ obstruction
and severe pyelocalyceal dilation had poorer results than those with mild
pyelocalyceal dilation.
Key words:
kidney; kidney pelvis; ureteral obstruction; ureteral stricture
Int Braz J Urol. 2002; 28: 302-10
INTRODUCTION
Pyeloplasty
remains the gold standard technique for treating ureteropelvic junction
obstruction (UPJ) (1). Success rate for this technique, in different series,
ranged between 90 and 95% (2). Although long-term results are good, this
procedure has some drawbacks: it is an invasive method, causes severe
postoperative pain, convalescence takes a long time, and patient will
have with a permanent cutaneous scar.
Endourologic techniques constitute an alternative
for open surgery (3). The treatment of the UPJ obstruction by percutaneous
access was performed for the first time in 1983. The procedure was then
known as percutaneous pyelolysis (4). In 1986, it was acknowledged throughout
the world as antegrade or percutaneous endopyelotomy (5). This technique
requires a percutaneous access and one possible complication directly
related to this method is bleeding (6). Investigators published, in 1983
in the urologic literature, their preliminary experience with endopyelotomy,
performed by retrograde access using a newly developed catheter called
Acucise™ (7). The treatment of UPJ strictures with the Acucise™
catheter by retrograde access is considered a minimally invasive new alternative
therapy, with encouraging results (8,9). In the present study, we report
our experience in managing ureteropelvic obstruction with the Acucise™
catheter.
PATIENTS AND METHODS
During
the time period of May 1997 to April 1999, 30 patients with UPJ obstruction
were treated by Acucise™ endopyelotomy. Ten patients were male, and
20 were female. Patients’ ages ranged from 8 to 75 years old (mean
= 36.2), Figure-1. The study excluded patients with UPJ obstruction due
to malignancies, previous radiotherapy, and retroperitoneal fibrosis.
Diagnostic suspicion was made in 26 patients
based only on clinical symptoms. Four were asymptomatic, and the diagnostic
suspicion was reached analyzing tests performed for other indications.
Diagnosis was confirmed based on results of intravenous urography and
diuretic renography. Clinical symptoms were back pain in 19 patients,
renal colic in 6, and abdominal pain in 1 (Table-1).

All patients underwent intravenous urography,
and in 27 patients, a diuretic renography was also performed. Twenty-four
patients had primary UPJ stricture, and in 6 the obstruction was secondary.
Of the 6 patients presenting secondary stricture, 5 had suffered previous
surgeries for removal of renal calculi. One patient with secondary obstruction
had undergone pyeloplasty 7 years before, due to primary UPJ obstruction.
All patients had a complete blood test pre-operatively, with measurement
of urea and creatinine, clotting factors, type I urinalysis and urine
culture with sensibility tests. No patients with urinary tract infections
were submitted to surgery.
Patients were informed that if failure occur,
open surgery or laparoscopic pyeloplasty might be necessary. They were
also told that in case of hemorrhage, its management could include blood
transfusion, arteriography with selective embolization of the damaged
blood vessel, surgical investigation, and even nephrectomy.
A broad-spectrum antibiotic was given to
patients on the day prior to surgery. Endopyelotomy was performed in all
patients, using the Acucise™ catheter, with a diameter of 5F in its
extremity. Twenty-seven patients, for whom the retrograde access was adopted
for the procedure, were given epidural or spinal anesthesia, the remaining
3 were submitted to antegrade endopyelotomy and received general anesthesia.
Lithotomy position was used for the 27 patients that were submitted to
retrograde endopyelotomy, and prone position for 3 patients that underwent
antegrade endopyelotomy.
For 3 patients with UPJ obstruction and
renal calculus, the antegrade access was chosen for the procedure. First,
a percutaneous nephrolithotripsy was performed, followed by endopyelotomy.
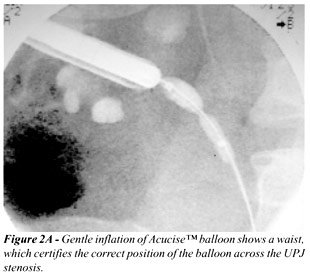
The Acucise™ catheter balloon was positioned at the site of the obstruction,
under direct and fluoroscopic vision, and the stenotic ring was visualized.
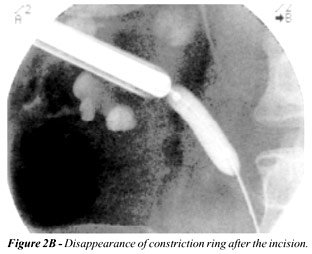
The incision was made under direct vision, disappearance of the stenotic
ring was visualized on the fluoroscopic image (Figure-2). Afterwards,
a 7F double-J catheter was inserted.
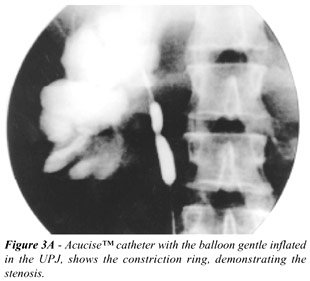
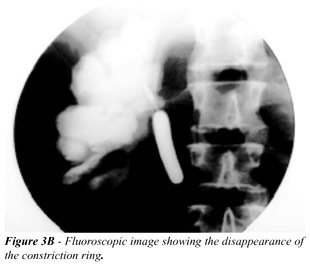
In 27 patients, the access was retrograde
or ascendant, which is the standard approach. The surgical technique performed
was similar to one described in detail by other authors (9,10,12). The
stricture is identified as a constriction ring or as a sandglass shape,
once the balloon is inflated (Figure-3A). Simultaneously, the stenotic
segment was incised using an electrocautery; the balloon was then inflated
with 2.2 cc of distilled water and contrast medium. After incision, it
is observed the disappearance of the constriction ring (Figure-3B). The
balloon was maintained inflated for 10 minutes to prevent bleeding. A
7F double-J catheter was placed. A Foley vesical stent was passed at the
end of the procedure and left in place for 24 hours. The vesical stent
avoids urine leakage at the site of the incision. The procedure was thoroughly
monitored by fluoroscopy. Time of permanence of the double-J catheter
was 6 weeks; removal was performed under local anesthesia as an outpatient
procedure. Success was defined considering both radiographic patency and
symptomatic relief of symptoms.
Clinical evaluation was carried-out after
16 weeks. Patients were asked whether the symptoms were worse, had improved,
disappeared or had remained unchanged.
Imaging studies were conducted 16 weeks
following surgery, and comprised an intravenous urography and a diuretic
renography.
The mean operative time for the antegrade
approach ranged from 200 to 220 minutes (mean = 210). The time for the
retrograde access procedure ranged between 30 and 80 minutes (mean = 52).
For procedures performed using the retrograde
access, postoperative hospital stay was approximately 24 hours. For percutaneous
antegrade endopyelotomies and nephrolithotripsies, hospital stay was about
3 days.
Postoperative follow-up ranged between 4
and 20 months. The mean follow-up time was 11.8 months.
RESULTS
Of
26 patients who reported lumbar pain during preoperative period, considering
pain as a characteristic symptom, 23 became asymptomatic following the
procedure.
Of 24 patients with primary UPJ obstruction,
20 had pain before the procedure and 19 became asymptomatic during postoperative
follow-up. The 6 patients with secondary UPJ obstruction had pain before
surgery, 4 of them became asymptomatic during follow-up.
During postoperative evaluation, intravenous
urography was performed in all patients. In 26 the outcome was good, considering
lower pyelocalicial dilation and patency of ureteropelvic junction. No
changes could be detected in 4 patients, and this was considered failure
(Table-2).
Twenty-seven patients were submitted to
a diuretic renography. For 23 there was evidence of a curve in radioactive
material excretion without obstruction, and in 4 an obstructive pattern
was observed.
Twenty-one patients with mild pyelocalyceal
dilation had good results. Among 9 patients presenting severe pyelocalyceal
dilation, 5 experienced good results (55.5%), and 4 remained unchanged
(44.5%) (Table-3). These percentages indicate a statistically significant
difference (p=0.005).
In analyzing the 24 patients with primary
UPJ obstruction, 22 had good outcome (91.6%). Of 6 patients with secondary
UPJ obstruction, outcome was good in 4 (66.7%). These results showed no
statistically significant difference (p=0.169) (Table-4).
During evaluation of 21 patients presenting
with mild pyelocalyceal dilation, it was observed that all patients had
good results, regardless the primary or secondary etiology of the stricture.
However, among 9 patients with severe pyelocalyceal dilation, 6 had primary
obstruction and in 3 the etiology of the obstruction was secondary. Among
6 patients with primary stricture, good results were achieved in 4 (66.6%).
Of 3 patients with secondary obstruction, only 1 showed good results (33.4%).
This data express a statistically significant difference (Table-5).
Three patients had acute pyelonephritis
during postoperative period. None of them had severe bleeding, and did
not require any complementary procedure.
DISCUSSION
The
Acucise™ catheter was designed to perform an precise incision of
ureteropelvic junction under fluoroscopic guidance. Early studies on the
use of the Acucise™ catheter in treating UPJ obstruction were reported
in 1993. From that time on, UPJ and ureteral obstruction at any site could
be managed by this method. This procedure is performed endoscopically,
and is considered a minimally invasive surgery (7,9,10). Both primary
and secondary strictures can be treated, and the success rate is similar
in the 2 groups, showing long lasting results (11).
Three patients in the present series had
renal calculi and UPJ obstruction; we used the antegrade access for simultaneous
management of calculi and obstruction. Kidney puncture was performed in
an intermediate or upper calyceal group to obtain a better access to the
UPJ. In 3 patients, it was possible to remove all the calculi and perform
Acucise™ endopyelotomy. The antegrade approach method was carried
out using a video camera, which allowed visualization of UPJ before and
after incision. We were convincingly shown that the incision of the stricture
was thorough and complete. The percutaneous access and subsequent insertion
of a percutaneous tube imply some risks and discomfort.
Four patients were diagnosed during investigation
of other pathologies. Two had mild pyelocalyceal dilation and 2 had severe
pyelocalyceal dilation. In many patients an UPJ obstruction can be diagnosed
incidentally, as symptoms may be absent. Even when present, symptoms are
atypical and intermittent (12,13).
Regeneration of ureter occurs within a maximum
period of 40 days. In a study involving 13 patients with UPJ obstruction,
treated by Acucise™ endopyelotomy, and followed up for a mean time
period of 17 months, it was observed that recurrence of obstruction takes
place during the first three months (14).
Severe pyelocalyceal dilation, compression
of UPJ by an anomalous vessel and obstruction exceeding 2cm in length
are the unfavorable factors related to the outcome of endopyelotomy (13).
The success rate for endopyelotomy in patients
with severe pyelocalyceal dilation is approximately 60% (13,15). The low
pelvic pressure causing difficulty in pyelocalyceal voiding may be an
explanation for this outcome. For a better drainage of urine, the UPJ
must occupy the lowest position in the renal pelvis. In patients with
severe pyelocalyceal dilation, the most caudal region of renal pelvis
can exert a compression on UPJ causing a functional obstruction (13,16).
Some authors recognize endopyelotomy as
the first-line therapeutic option, even for patients with severe pyelocalyceal
dilation, since this is a minimally invasive procedure, with outcomes
that cannot be neglected. If recurrence of the obstruction takes place,
pyeloplasty is indicated; in this case, the previously performed endopyelotomy
does not preclude the procedure (13,17).
There are studies showing better outcomes
of retrograde Acucise™ endopyelotomy for secondary than for primary
obstruction. The authors are convinced that there is a lower incidence
of anomalous vessels compressing the UPJ in secondary obstruction than
in primary strictures. Some authors also believe that urine extravasation
into the retroperitoneum is lower in secondary obstruction due to the
existence of local periureteral fibrosis which contributes to better outcome.
A great deal of urine extravasation into retroperitoneum can lead to the
development of further local fibrosis, increasing the possibility of obstruction
recurrence (18).
Digital angiography, endoluminal ultrasonography,
and spiral computed tomography have been employed with the purpose of
detecting anomalous blood vessels that cross the UPJ. Digital angiography
and transluminal ultrasonography are invasive and expensive procedures,
whereas helical computed tomography is not considered an invasive investigation,
but the cost is high for routine indication (19).
In 1993, was published a study with 146
autopsy kidneys investigated. Authors analyzed the anatomical correlation
between blood vessels and UPJ. This study demonstrated that even in normal
kidneys there are blood vessels crossing UPJ. They also found prominent
vessels (artery or vein) crossing the anterior and posterior aspects of
UPJ in 65% and 6.2% of cases, respectively. It was evidenced that the
lateral region of the UPJ is the site with lesser possibility of presenting
an anomalous vessel (20).
Bleeding following retrograde Acucise™
endopyelotomy is not very frequent. The requirement for blood transfusion
ranged between 1 and 3%. When serious bleeding occurs, blood transfusion
and emergency arteriography are recommended, with selective embolization
of the injured vessel (21).
Results of antegrade endopyelotomy using
a cold knife and retrograde Acucise™ endopyelotomy were compared
in several studies. Findings indicated that retrograde endopyelotomy performed
with the Acucise™ catheter is better tolerated, operative time is
shorter, postoperative hospital stay, as well as convalescence, is reduced.
Complications are uncommon and occur with a similar frequency in both
groups (10).
In our series 2 children were treated by
retrograde access. The procedure was successful at its first attempt for
both. Postoperative outcome was good in these pediatric patients.
In a recent article it has been reported
that 2 male patients, aged 4 and 6 years, were managed by retrograde pyelotomy
using the Acucise™ catheter. The authors had no difficulties, and
no complications occurred pre- or postoperatively. A short follow-up period
revealed a good outcome in both children (9).
In a study involving 45 patients, the authors
have compared pyeloplasty with 3 minimally invasive surgical modalities:
antegrade endopyelotomy, retrograde Acucise™ endopyelotomy and laparoscopic
endopyelotomy. Outcome was good in 100% of patients managed by laparoscopic
pyeloplasty, 78% who underwent retrograde endopyelotomy using the Acucise™
catheter (22), and 77% submitted to antegrade cold knife endopyelotomy.
A comparative study was carried out to investigate tolerance regarding
minimally invasive techniques used in the treatment of UPJ obstruction.
As parameters the authors considered operative time, doses of narcotics
necessary during postoperative period, mean hospital stay, and time to
recovery. According to their report, retrograde Acucise™ endopyelotomy
was associated with the best tolerance (22).
CONCLUSIONS
Endopyelotomy with the Acucise™ catheter showed to be a simple and safe procedure, being a minimal invasive alternative to pyeloplasty. Patients with UPJ obstruction and mild pyelocalyceal dilation, independent of etiology, had success. Patients with UPJ obstruction and severe pyelocalicial dilation had the worse results.
REFERENCES
- Clayman RV, McDougall EM, Nakada SY: Strictures of the Upper Urinary Tract. In: Wash PC, Retik AB, Vaughan ED, Wein AJ (eds.). Campbell’s Urology, 7th ed. Philadelphia, WB Saunders, 1998; vol. 3, p. 2841-74.
- Schaeffer AJ, Grayhack JT: Surgical Management of Ureteropelvic Junction Obstruction. In: Walsh PC, Gittes RF, Perlmutter AD, Stamey TA (eds.). Campbell’s Urology, 5th ed. Philadelphia, WB Saunders, 1986; p. 2505-16.
- Lechevallier E, Eghazarian C, Ortega JC, André M, Gelsi E, Coulange C: Retrograde Acucise™ endopyelotomy: Long-term results. J Endourol. 1999. 13: 575-80.
- Wickham, JEA, Kellet MJ: Percutaneous pyelolysis. Eur Urol. 1983, 9: 122-4.
- Badlani G, Eshghi M, Smith AD: Percutaneous surgery for ureteropelvic junction obstruction (endopyelotomy): Technique and early results. J Urol. 1986; 135: 26-30.
- Motola JA, Badlani GH, Smith AD: Results of 212 consecutive endopyelotomies: A 8 year follow up. J Urol. 1993. 149: 453-6.
- Chandhoke PS, Clayman RV, Stone AM, McDougall EM: Endopyelotomy and endoureterectomy with the Acucise™ ureteral cutting balloon device: Preliminar experience. J Endourol. 1993; 7: 45-51.
- Cohen TD, Gross MB, Preminger GM: Long-term follow-up of Acucise™ incision of ureteropelvic junction obstruction and ureteral strictures. Urology. 1996; 47: 317-23.
- Faerber GJ, Richardson, TD, Farah N: Retrograde treatment of ureteropelvic junction obstruction using the ureteral cutting balloon catheter. J Urol, 1997; 157: 454-8.
- Preminger GM, Clayman RV, Nakada SY: A multicenter clinical trial investigating the use of a fluoroscopically controlled cutting balloon catheter for the management of ureteral and ureteropelvic junction obstruction. J Urol. 1997; 157: 1625-9.
- Banerjee GK, Ahlawat R, Dalela D: Endopyelotomy and pyeloplasty: face to face. Eur Urol. 1994; 26: 281-5.
- Van Cangh PJ, Wilmart JF, Opsoner RJ: Long-term results and late recurrence after endopyelotomy: A critical analysis of prognostic factors. J Urol. 1994; 151: 934-7.
- Danuser H, Ackermann DK, Dominique B: Endopyelotomy for primary ureteropelvic junction obstruction: Risk factors determine the success rate. J Urol. 1998; 159: 56-61.
- Gill HS, Liao JC: Pelvi-ureteric jun ction obstruction treated with Acucise™ retrograde endopyelotomy. Br J Urol. 1998; 82: 8-11.
- Van Cangh PJ, Nesa S, Galeon M: Vessels around de ureteropelvic junction: Significance and imaging by conventional radiology. J Endourol. 1996; 10: 111-9.
- Anderson KR, Weiss RM: Physiology and evaluation of ureteropelvic junction obstruction. J Endourol. 1996; 10: 87-90.
- Brito AH, Mitre AI, Arap S: Endopielotomia com cateter Acucise™. J Bras Urol. 1999; 25: 30-5.
- Gelet A, Combe M, Ramackers JM: Endopyelotomy with Acucise™ cutting balloon device. Eur Urol. 1997; 31: 389-93.
- Nakada SY, Wolf JS, Brink JA: Retrospective analysis of the effect of crossing vessels on successful retrograde endopyelotomy outcomes using spiral computerized tomography angiography. J Urol. 1998; 159: 62-5.
- Sampaio FJ, Favorito L: Ureteropelvic junction stenosis: vascular anatomic background for endopyelotomy. J Urol. 1993; 150: 1787-91.
- Streem SB, Geisinger MA: Prevention and management of hemorrhage associated with cautery wire balloon incision of ureteropelvic junction obstruction. J Urol. 1995; 153: 1904-6.
- Brooks JD, Kavoussi LR, Preminger GM: Comparison of open and endourologic approaches to the obstructed ureteropelvic junction. Urology. 1995; 46: 791-5.
______________________
Received: March 11, 2002
Accepted after revision: July 6, 2002
_______________________
Correspondence address:
Dr. Artur Henrique Brito
Rua Barata Ribeiro, 414 /36
Sao Paulo, SP, 01308-000, Brazil
Fax: + 55 11 3218-8285
E-mail: arturbrito@uol.com.br
The
authors review their results using the Acucise™ balloon catheter
for management of both primary and secondary UPJ obstruction, in both
a retrograde and, in a few patients, antegrade fashion. A standard technique
has been developed and well described previously, and a similar technique
followed by the authors. With a mean follow-up of just under one year,
the authors report an 86% “success” rate which is slightly higher
than that reported in the literature, but consistent with previous reports.
The authors have done an excellent job evaluating
the postoperative result both symptomatically (subjectively) and objectively
with follow-up intravenous pyelography and, in the great majority of the
patients, diuretic renography. However, the definition of success is still
somewhat unclear, as it is with most similar papers in the literature.
Success for managing ureteropelvic junction obstruction cannot be defined
as either subjective or objective success alone. The goal of the procedure
is complete symptomatic relief and freedom from functional obstruction.
As such, success should only be defined as relief of symptoms combined
with radiographic evidence of a non-obstructed system. It is unclear how
many of these patients in this study fit both categories, that is, those
that are both free of pain and free of any residual functional obstruction.
Another potential explanation for the relatively
high success rate is the relatively short follow-up duration. Follow-up
was less than two years in all patients, and the mean overall follow-up
was less than one year. In fact, while most failures of this approach
will be apparent within one year, with time, success rates can only diminish
as more patients suffer recurrent pain and obstruction. As such, as the
mean follow-up in this study group increases in time, more failures will
clearly become evident.
The authors have appropriately managed the
majority of their patients with a retrograde approach and utilized a percutaneous
antegrade approach only for those with concomitant upper tract stones,
such that the stones and the UPJ obstruction could be managed simultaneously.
However, one might question whether the use of the Acucise™ balloon
was appropriate during a percutaneous procedure. Percutaneous endopyelotomy
has been well described by others using either a cold knife or an electrosurgical
incision with either a Bugbee electrode or Collins’ knife. The procedure
is easily performed under direct vision and the need to use the Acucise™
balloon with its attendant increased expense does not seem clearly justified.
Finally, while the technique and results
reported here are consistent with those on the literature, suggesting
an ongoing role for the use of the Acucise™ balloon, at most centers,
patients who otherwise might have been managed with the Acucise™
balloon are now being managed with a direct vision ureteroscopic approach.
In most cases this is performed using a Holmium laser for the incision,
though a small Bugbee electrosurgical incision provides comparable results.
In this age of smaller semi-rigid and flexible ureteroscopes, the ability
to reach the ureteropelvic junction without complications has become a
routine part of urologic endoscopy. With it, the ability to make the endopyelotomy
incision under direct visual control is quickly relegating the use of
a fluoroscopically guided hot-wire balloon incision to more of a “historical”
interest.
Dr. Stevan B. Streem
Section of Stone Disease and Endourology
The Cleveland Clinic Foundation
Cleveland, Ohio, USA