INFANTILE
BLADDER RUPTURE DURING VOIDING CYSTOURETHROGRAPHY
(
Download pdf )
ABDOL M. KAJBAFZADEH, PARISA SAEEDI, ALI R. SINA, SEYEDMEHDI PAYABVASH, AMIRALI H. SALMASI
Pediatric Urology Research Center, Department of Urology, Children’s Hospital Medical Center, Tehran University of Medical Sciences, Tehran, Iran
ABSTRACT
Bladder rupture is rare during infancy and most of reported cases had urethral obstruction or neurogenic bladder. We report two cases of infantile bladder rupture during voiding cystourethrography (VCUG). This report reinforces the criteria for proper VCUG imaging procedure. Consideration of expected bladder volume for body weight, and close monitoring of bladder pressure and injection speed could prevent such complications.
Key
words: bladder; children; diagnostic imaging; rupture; iatrogenic
Int Braz J Urol. 2007; 33: 532-5
INTRODUCTION
Voiding cystourethrography (VCUG) is widely applied for the radiological evaluation of the bladder and urethra in children. Bladder rupture during VCUG is exceedingly rare (1). We present two infants with iatrogenic bladder rupture during VCUG performed by radiology staffs in two district hospitals. These infants were referred to our center for further management.
CASE REPORTS
Case
#1 - A 10-day-old boy, weighing 3.2 kg, was referred to nephrologists
with history of prenatal hydronephrosis. On day 7 after birth, ultrasonographic
exam confirmed bilateral hydroureteronephrosis, which was severe on the
left side and mild on the right side. VCUG was requested to evaluate a
possible vesicoureteral reflux (VUR). A 6F feeding tube was inserted into
the urethra and contrast media was injected using a 50-mL syringe, under
fluoroscopic guide. During the first filling cycle, severe left side VUR
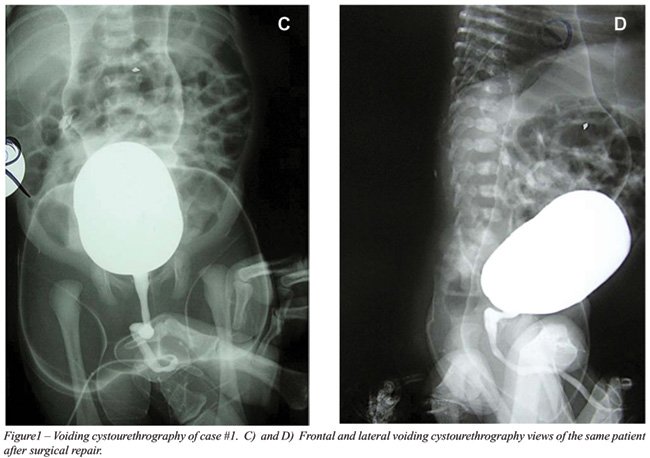
appeared following injection of 15 mL of contrast media (Figure-1) and
the right VUR appeared in volume of 35 mL. However, the radiographer continued
the instillation until the intraperitoneal bladder rupture occurred in
volume of 60 mL (Figure-1). The baby was referred to urologist and immediately
underwent abdominal exploration through a Pfannenstiel incision. The bladder
dome was the site of a 2 cm long rupture. The peritoneal cavity was washed
with saline and the bladder was closed in two layers using 4-0 polyglactin
suture. A Malecot catheter was inserted in the bladder as suprapubic tube.
A mini-vacuum closed drain was left in the perivesical space. The post-operative
course was complicated by prolonged urine leakage from the site of suprapubic
catheter extracted on the 14th postoperative day. The child
was referred to our institution for further management. A 6F Foley urethral
catheter was inserted. After 7 days, the leakage was stopped and the catheter
was removed on the 24th postoperative day. The patient was
discharged 3 days later with good condition and prescription of prophylactic
antibiotic (Figure-1).

Case #2 - A 9-month old female infant, weighing
7 kg, was referred to a radiologist for VCUG at a district hospital from
a different province. Medical problems included urinary tract infection
and failure to thrive. Contrast media was injected through an 8F urethral
feeding tube under fluoroscopic guide. The radiographer instilled 100
mL of contrast media using a 50-mL syringe, during the first filling cycle.
Speed of injection, bladder pressure and volume were not recorded. While
reviewing the images, the radiologist discovered bladder perforation.
She was taken to the operating room and underwent abdominal exploration.
The bladder was exploded at dome with a 3 cm length. The site of perforation
was closed in two layers using absorbable 4-0 polygalactin suture. A small
Penrose drain was left in perivesical space and a 10F catheter was left
per urethra. Post-operative course of the patient was uneventful and she
was discharged one week later and referred to our clinic for further evaluation.
Follow-up VCUG showed no leakage or reflux.
COMMENTS
Infantile
bladder rupture is rare (2) and only 17 cases have been reported between
1956 and 1985 (3). The main predisposing factors include posterior urethral
valves and neurogenic bladder followed by bladder outlet obstruction from
other etiologies and trauma (3). Few cases of iatrogenic bladder perforation
have been reported in children following diagnostic and therapeutic procedures
(3,4). To our knowledge this is the second report of infantile bladder
rupture during VCUG (2).
There was none of the above-mentioned risk
factors in our cases; however, inaccurate imaging procedure seems to be
the main cause of perforation. In order to perform a safe and perfect
VCUG, radiologists must pay attention to some factors such as bladder
volume, style of contrast media instillation and patient conditions (underlying
urinary disease) (1). Two formulae have been proposed for bladder volume
estimation in children with regards to their weight and age (4,5); age
< 2 years - bladder volume (mL) = weight (kg) × 7, age > 2
years - bladder volume (mL) = [age (years) + 2] × 30.
Proper catheter insertion, fluoroscopic
guide, pressure and number of filling cycle should be considered in styles
of instillation (1). To avoid pressure overload, hand injection of contrast
material must not be used and the contrast container should not be placed
higher than 60 cm from the patient. More than two cycles of filling does
not appear to be necessary (1,6). The underlying urinary system disease
is another important factor. In our cases, the bladder volume and pressure
were not considered and the contrast media was instilled directly by syringe.
Management of infantile bladder rupture
should be individualized. In the review by Trulock et al. (3), the majority
of reported neonates were treated with abdominal exploration and repair
of the bladder leakage site; however some of the patients would be managed
by the use of vesicostomy or urethral catheter alone.
In conclusion, during VCUG, it is important
to consider the patient underlying disorder and expected bladder volume
for age as well as to avoid hand injection of contrast material and placing
the contrast container more than 60 cm higher than the patient. Moreover,
in order to prevent high-pressure voiding in premature infants, it has
been recommended to use small caliber and balloon-less feeding catheters
that would not occlude the bladder neck during voiding.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Agrawalla S, Pearce R, Goodman TR: How to perform the perfect voiding cystourethrogram. Pediatr Radiol. 2004; 34: 114-9.
- Wosnitzer M, Shusterman D, Barone JG: Bladder rupture in premature infant during voiding cystourethrography. Urology. 2005; 66: 432.
- Trulock TS, Finnerty DP, Woodard JR: Neonatal bladder rupture: case report and review of literature. J Urol. 1985; 133: 271-3.
- O’Brien WJ, Ryckman FC: Catheter-induced urinary bladder rupture presenting with pneumoperitoneum. J Pediatr Surg. 1994; 29: 1397-8.
- Koff SA: Estimating bladder capacity in children. Urology. 1983; 21: 248-52.
- Jequier S, Jequier JC: Reliability of voiding cystourethrography to detect reflux. AJR Am J Roentgenol. 1989; 153: 807-10.
____________________
Accepted after revision:
April 27, 2007
_______________________
Correspondence
address:
Dr. A.M. Kajbafzadeh
No. 36, 2nd Floor, 7th Street
Saadat-Abad, Ave. Tehran 19987, Iran
Fax: + 98 21 2206-9451
E-mail: kajbafzd@sina.tums.ac.ir
EDITORIAL COMMENT
The authors of this manuscript present two cases of iatrogenic bladder rupture in infants undergoing voiding cystourethrograms. This radiographic study is one of the most common imaging studies ordered in children and needs to be performed safely and reliably. Those of us who work in dedicated children’s hospitals take this for granted. However, the cases reported in this series were performed by radiologists clearly unfamiliar with proper technique as nicely outlined by the authors. It is important to remember that the peritoneum drapes quite anteriorly in small children thus making a rupture very likely to be intraperitoneal, as in these two cases, and therefore surgical exploration is required.
Dr. Lane
S. Palmer
Chief, Pediatric Urology
Schneider Children’s Hospital
North Shore-Long Island Jewish Health System
New York, NY, USA
E-mail: lpalmer@nshs.edu