RETROPERITONEOSCOPY
FOR TREATMENT OF RENAL AND URETERAL STONES
(
Download pdf )
RODRIGO S. SOARES, PEDRO ROMANELLI, MARCOS A. SANDOVAL, MARCELO M. SALIM, JOSE E. TAVORA, DAVID L. ABELHA JR
Section of Urology, Hospital da Previdência dos Servidores do Estado de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
ABSTRACT
Objective:
To assess the efficacy of retroperitoneoscopy for treating stones in the
renal pelvis and proximal ureter.
Materials and Methods: In the period from
August 2003 to August 2004, 35 retroperitoneoscopies for treatment of
urinary stones were performed on 34 patients. Fifteen patients (42%) had
stones in the renal pelvis, and in 2 cases, there were associated stones
in the upper caliceal group. Twenty patients (58%) had ureteral stones,
all of them located above the iliac vessel. Twenty-five patients (71%)
had previously undergone at least one session of extracorporeal lithotripsy
and 8 patients (26%) also underwent ureteroscopy to attempt to remove
the stone. Eight patients underwent retroperitoneoscopy as a primary procedure.
Stone size ranged from 0.5 to 6 cm with a mean of 2.1 cm.
Results: Retroperitoneoscopy was performed
by lumbar approach with initial access conducted by open technique and
creation of space by digital dissection. We used a 10-mm Hasson trocar
for the optics, and 2 or 3 additional working ports placed under visualization.
Following identification, the urinary tract was opened with a laparoscopic
scalpel and the stone was removed intact. The urinary tract was closed
with absorbable 4-0 suture and a Penrose drain was left in the retroperitoneum.
In 17 patients (49%), a double-J stent was maintained postoperatively.
Surgical time ranged from 60 to 260 minutes with a mean of 140 minutes.
The mean hospital stay was 3 days (1-10 days). The mean length of retroperitoneal
urinary drainage was 3 days (1-10 days). There were minor complications
in 6 (17.6%) patients and 1 case of conversion due to technical difficulty.
Thirty-three patients (94%) became stone free.
Conclusion: Retroperitoneoscopy is an effective,
low-morbidity alternative for treatment of urinary stones.
Key
words: kidney calculi; ureteral calculi; surgery; laparoscopy;
retroperitoneal space
Int Braz J Urol. 2005; 31: 111-6
INTRODUCTION
Recent advances in extracorporeal lithotripsy and endoscopic techniques have made open surgery infrequent for treatment of urinary stones. However, patients with large impacted stones, especially those located in the proximal ureter, pose a challenge for treatment, often requiring multiple interventions. In such cases, open surgery remains a good, cost-effective alternative for resolution. The recent development of laparoscopic surgery has broadened the therapeutic options for several pathologies. The laparoscopic ureterolithotomy was initially described by Wickhan (1) in 1979, and more widely divulged since the early 1990s by Gaur (2), using the retroperitoneoscopic access. The present study reports the experience with retroperitoneoscopic ureterolithotomy and pyelolithotomy.
PATIENTS AND METHODS
Over
the period from August 2003 to August 2004, 34 patients ranging from 14
to 65 years of age (mean 32 years) underwent 35 retroperitoneoscopic interventions
for removal of urinary stones. Nineteen patients were male and 15 were
female. Twenty-four presented microscopic hematuria and/or lumbar pain,
4 patients had recurrent urinary infection and 5 patients were asymptomatic.
One patient presented obstructive acute renal failure with anuria and
anasarca due to bilateral stones.
In all patients, the diagnosis was confirmed
with imaging exams (plain abdominal x-ray, ultrasonography and excretory
urography or abdominal computerized tomography). Twenty-four patients
presented moderate or more pronounced hydronephrosis due to the presence
of stones. Two patients presented ureteropelvic junction stenosis with
associated stones. Two patients had complete ureteropelvic duplicity with
ureteral stones in the upper collecting system. Twenty-nine patients had
radiopaque stones and 5 had radiolucent ones. Stones were located on the
right side in 17 patients, on the left side in 16 patients, and 1 patient
had bilateral lithiasis.
Among the 34 patients, 31 had a single stone
and 3 had 2 or more stones or stone fragments. Twenty patients had ureteral
stones, with 14 located in the proximal ureter and 6 located in the middle
ureter. Fifteen patients presented renal stones, with 13 cases of single
pelvic stones and 2 cases of pelvic stones associated with stones in the
upper caliceal group. Twenty-five patients had previously undergone at
least 1 session of extracorporeal lithotripsy, and 7 patients also underwent
ureteroscopy in an attempt to remove the stone. One patient underwent
ureteroscopy only, which was unsuccessful. In 8 patients, retroperitoneoscopy
was indicated as the primary treatment. Eight patients presented previously
inserted double-J stents. One patient had a nephrostomy. Stone size ranged
from 0.5 cm to 6 cm in diameter (mean 2.1 cm).
The main indication for laparoscopy was
as an alternative to open and/or percutaneous surgery following failure
of extracorporeal lithotripsy and/or ureterolithotripsy. The condition
for indicating retroperitoneoscopy for ureteral stones was a location
above the iliac vessels, while the presence of an extra-renal or dilated
pelvis provided the condition for pelvic stones. The procedure was also
indicated in 2 cases with stones located in the upper calyx due to anatomical
aspects that favored extraction through the renal pelvis. Two patients
with UPJ stenosis underwent retroperitoneoscopic pyeloplasty during the
same surgical procedure. No patient presented previous lumbotomy. The
data for study analysis were collected retrospectively. All patients signed
an informed consent term.
Surgical Technique
The
procedure was a lumbar retroperitoneoscopic under general anesthesia in
all patients. In 5 cases, a double-J stent was positioned in retrograde
way during the immediate preoperative period. Patients were positioned
in the classic lumbotomy position with hyperextension. Access to the retroperitoneal
space was obtained with the open technique through a 1.5-mm subcostal
incision under the extremity of the 12th rib and muscle divulsion up to
the aponeurosis of the transverse muscle, which was then opened, and the
fascia transversalis, identifying the pre-renal fat. The creation of a
working space in the retroperitoneum was performed by digital dissection,
displacing the peritoneum medially without using a balloon. A Hasson trocar
was inserted in this space and fixed to the musculature with a purse-string
suture in order to avoid air leakage and development of subcutaneous emphysema,
and CO2 insufflation was performed until reaching 12-mm Hg tension. We
used 0-degree optics and, when needed, the working space was completed
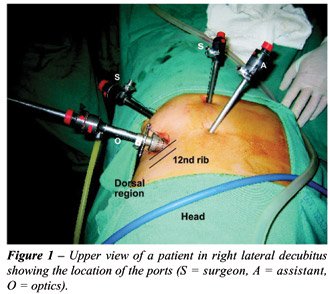
using the optics under visualization. Two additional trocars were placed
under visualization; a 5-mm trocar on the hemiclavicular line just above
the iliac spine and caudally to the optics port, and a 5- or 10-mm trocar
posterior to the optics at the posterior axillary line, forming a triangle.
Eventually, when retraction was required, another 5-mm trocar was placed
at an anterior position at the hemiclavicular line just below the costal
margin (Figure-1).
The ureter was initially identified in its
middle portion within the retroperitoneal fat and dissected up to the
level of the UPJ. Identifying the stone was also relatively easy in cases
with upstream dilation of the urinary tract. Two cases required the use
of radioscopy. The accurate location of the intra-ureteral stone was achieved
by palpation with laparoscopic forceps.
In the majority of cases, the urinary tract
was opened with a longitudinal incision using a laparoscopic scalpel.
At the beginning of our experience, due to the unavailability of tools,
the opening was performed using laparoscopic scissors or diathermy and
a metallic curve needle held by laparoscopic forceps. Stone extraction
was performed using laparoscopic forceps only. In both cases with stones
in the upper caliceal group, the stone was extracted with a rigid nephroscope
inserted through an Amplatz sheath placed at the incision site for the
optic port after removing the Hasson trocar. The nephroscope was guided
to the renal pelvis by a guide wire that had been previously positioned
through pyelotomy and the stone was removed using transnephroscopic forceps
under saline solution irrigation. In cases where it was feasible, the
stone was immediately removed from the cavity using the inner area of
one of the trocars without contacting the wall. Large stones were temporarily
kept in the retroperitoneal space and, at the end of the surgery, the
stone was introduced into a bag made out of a surgical glove and then
removed.
The double-J stent was positioned during
the surgical procedure in 9 cases, during the immediate peroperative period
by retrograde approach in 5 cases and during the peroperative period by
antegrade approach in 4, using a guide wire through one of the 5-mm ports.
The indication for inserting the stent in the peroperative period was
if there was complete obstruction of the urinary tract due to a long-term
impacted stone or the technical difficulty of achieving a satisfactory
closure of the renal pelvis or ureter at the beginning of our experience.
Suture of the urinary tract was performed
in all cases, except, due to technical difficulties, in one case of pyelolithotomy.
In the first 10 cases, closure was performed with single stitches using
non-absorbable 4-0 polyglycolic acid sutures; the other cases used 4-0
chromic catgut. Eventually the continuous suture was performed in wider
pyelotomies. A Penrose drain was placed in the retroperitoneum and exteriorized
through one of the port incisions, and was subsequently removed when the
drainage was lower than 30 mL/24 hours. The ureteral catheter was removed
on average 3 weeks after the procedure and a radiographic control was
performed around the 30th postoperative day.
RESULTS
Stone
removal using the retroperitoneoscopic approach was successfully accomplished
in 33 of the 35 interventions. In one case, conversion to open surgery
was required due to technical difficulties. In another case of ureteral
stone with a previously inserted double-J stent, it was impossible to
locate the stone even with radioscopic aid. This patient subsequently
underwent a new ureterosocopy, achieving stone removal.
Surgical time ranged from 60 min to 260
min (mean 140). Peroperative bleeding was negligible, except in 2 patients
that presented bleeding of approximately 500 mL due to damage to the left
gonadal vein and 1 parietal artery, respectively. In both cases, bleeding
was controlled without requiring conversion to open surgery. One patient
presented a voluminous retroperitoneal hematoma in the postoperative period,
which was treated conservatively. No case required blood transfusion,
the hospital stay ranged from 1 to 10 days (mean 3) and the follow-up
ranged from 2 to 12 months (mean 7). All patients became stone-free and
no case of urinary tract stenosis was observed during the follow-up.
The length of urinary drainage through the
Penrose drain ranged from 1 to 10 days (mean 3 days), being more prolonged
in cases where the urinary tract was not opened with laparoscopic scalpel,
in cases without double-J stent and in 1 case with double-J stent and
in 1 case where the pyelotomy was not sutured. In 2 cases with abundant
postoperative drainage, the postoperative insertion of a double-J stent
allowed the closure of the fistula in 1 day. Postoperative complications
occurred in 6 (17.6%) patients. Two patients presented an abscess at the
port site where the Penrose drain was exteriorized. One patient who had
previous nephrostomy developed urinary sepsis during the postoperative
period following inadvertent removal of the nephrostomy and improved after
inserting a retrograde ureteral catheter. One patient evidenced retroperitoneal
hematoma and was treated conservatively. One patient presented pain and
paresthesia in the ipsilateral lumbar region due to a thermal lesion of
the intercostal nerve during efforts to control the bleeding of the intercostal
artery, and was clinically managed. Another patient presented subcutaneous
emphysema due to subcutaneous insufflation of CO2 with no clinical repercussions.
COMMENTS
Despite
the development of extracorporeal lithotripsy and advancements in endoscopic
techniques for treatment of urinary stones, some patients still undergo
open surgery (3). The main surgical indications in our setting result
from failure and/or unavailability of minimally invasive techniques. The
recent advancement of laparoscopy in the urologic field has permitted
a new alternative for treatment of stones (4).
Traditionally the access for stone removal
in open surgery is achieved by retroperitoneal approach. Some authors
advocate laparoscopic surgery for managing stones using the intraperitoneal
approach (4-7) since it has the advantage of providing a larger working
space. The retroperitoneoscopic approach spread widely following the use
of a balloon for creating a working space in a study developed by Gaur
(2,8). This approach provides direct access to the urinary tract and avoids
manipulation and contact of urine with the intraperitoneal organs. The
main disadvantage of retroperitoneoscopic access is the smaller working
space, which renders reconstructive procedures such as suturing of the
urinary tract more difficult (8). In our experience, the use of a balloon
was not required for creating the retroperitoneal space. Using only digital
dissection and complementing the dissection with the optic itself when
required, we obtained a space that allowed us to fully perform the procedure
with satisfactory laparoscopic sutures. Positioning the surgeon’s
working ports caudally to the optics makes the procedure easier.
The lumbar retroperitoneoscopic approach
allows a fast and direct access to the urinary tract from the renal pelvis
to the ureter at the level of the iliac vessels. In favorable conditions,
it is possible to obtain access to stones located in caliceal groups,
especially the upper groups, through the renal pelvis. In 2 cases it was
possible to extract upper caliceal stones using a rigid nephroscope that
was inserted through an opening in the renal pelvis. Those cases had dilated
calices and wide infundibulum, which made the procedure easier. The combination
of laparoscopic and percutaneous nephrolithotripsy techniques has already
been described, especially for treating stones in ectopic kidneys (9).
However, the present study shows the possibility of successfully combining
these 2 techniques to extract caliceal stones in selected cases. The possibility
of accessing the stones using a transpelvic approach reduces the risk
of bleeding compared to the transparenchymal approach. This is an advantage
of retroperitoneoscopy over percutaneous nephrolithotomy. The selection
of patients with extra-renal and/or a dilated renal pelvis was fundamental
for obtaining good results with the retroperitoneoscopy. Another advantage
is the possibility of removing the stone intact with no fragmentation
and, thus, lower the risk of residual fragments. In all cases in this
series the stone was extracted intact, even in cases where the stone measured
more than 5 cm. At the moment, few studies have been published comparing
the classic open approach with retroperitoneoscopy (10). Other studies
are still required in order to assess each method’s advantages;
however, the advancement in laparoscopic techniques and instruments enables
us to widen the applications of retroperitoneoscopy (11,12).
Flexible urethroscopes or even flexible
cystoscopes using lasers (13-15) can also be used as a resource for application
by retroperitoneoscopic approach, similarly to what was performed in our
study with the rigid nephroscope, thus increasing the device’s scope
and the chances of success in selected cases.
Whether to use the ureteral catheter or
not is a controversial issue in urinary stone surgery (16). The presence
of a double-J stent makes identification of the ureter in the retroperitoneum
easier, however it makes the identification of the stone difficult since
it reduces the dilation of the urinary tract, and they can be easily mistaken
because of the stent’s rigidity. In one case from this series, in
a patient with a radiolucent ureteral stone, the presence of a previously
inserted double-J stent prevented the stone from being located.
In cases with anatomic changes to the urinary
tract, the laparoscopy represents a safe and effective alternative to
endoscopic procedures, which are often laborious and risky in such cases.
In 2 cases with pyeloureteral duplicity, the laparoscopic access enabled
easy localization and extraction of the stone after ureteroscopy efforts
had been frustrated. Similarly, in 2 cases with ureteropelvic junction
stenosis associated with stones in the dilated pelvis, laparoscopy enabled
easy stone extraction, and reconstruction with pelvic reduction, reproducing
the conventional open surgery (17).
Laparoscopy is a method that reproduces
the steps of open surgery and can be indicated as an alternative in cases
of therapeutic failure using less invasive methods (18,19). However, in
cases where the risk of failure using such method is high, such as anatomic
anomalies and voluminous and impacted ureteral stones, laparoscopy can
be indicated as a primary procedure (8). In cases of pelvic stones, the
retroperitoneoscopic pyelolithotomy is an alternative that allows the
removal of the intact stone with lower risk of residual fragments and
without requiring transparenchymal access, thus reducing the risk of bleeding.
REFERENCES
- Wickham JEA: The Surgical Treatment of Urinary Lithiasis. In Wickham JEA (ed.), Urinary Calculus Disease. New York, Churchill Livingstone. 1979; pp. 145-98.
- Gaur DD: Retroperitoneal laparoscopic ureterolithotomy. World J Urol. 1993; 11: 175-7.
- Assimos DG, Boyce WH, Harrison LH, McCullough DL, Kroovand RL, Sweat KR: The role of open stone surgery since extracorporeal shock wave lithotripsy. J Urol. 1989; 142: 263-7.
- Raboy A, Ferzli GS, Ioffreda R, Albert PS: Laparoscopic ureterolithotomy. Urology. 1992; 39: 223-5.
- Harewood LM, Webb DR, Pope AJ: Laparoscopic ureterolithotomy: the results of an initial series, and an evaluation of its role in the management of ureteric calculi. Br J Urol. 1994; 74: 170-6.
- Micali S, Moore RG, Averch TD, Adams JB, Kavoussi LR: The role of laparoscopy in the treatment of renal and ureteral calculi. J Urol. 1997; 157: 463-6.
- Keeley FX, Gialas I, Pillai M, Chrisofos M, Tolley DA: Laparoscopic ureterolithotomy: the Edinburgh experience. BJU Int. 1999; 84: 765-9.
- Gaur DD, Trivedi S, Prabhudesai MR, Madhusudhana HR, Gopichand M: Laparoscopic ureterolithotomy: technical considerations and long-term follow-up. BJU Int. 2002; 289: 339-43.
- Holman E, Toth C: Laparoscopically assisted percutaneous transperitoneal nephrolithotomy in pelvic dystopic kidneys: experience in 15 successful cases. J Laparoendosc Adv Sur Tech A. 1998; 8: 431-5.
- Goel A, Hemal AK: Evaluation of role of retroperitoneoscopic pyelolithotomy and its comparison with percutaneous nephrolithotripsy. Int Urol Nephrol. 2003; 35: 73-6.
- Gaur DD, Trivedi S, Prabhudesai MR, Gopichand M: Retroperitoneal laparoscopic pyelolithotomy for staghorn stones. J Laparoendosc Surg Tech A. 2002; 12: 299-303.
- Kaouk JH, Gill IS, Desai MM, Banks KL, Raja SS, Skarel M, et al.: Laparoscopic anathrophic nephrolithotomy: feasibility study in a chronic porcine model. J Urol. 2003; 169: 691-6.
- Chow GK, Patterson DE, Blute ML, Segura JW: Ureteroscopy: effect of technology and technique on clinical practice. J Urol. 2003; 170: 99-102.
- Kerbl K, Rehman J, Landman J, Lee D, Sundaram C, Clayman RV: Current management of urolithiasis: progress or regress? J Endourol. 2002; 16: 281-8.
- Landman J, Lee DI, Lee C, Monga M: Evaluation of overall cost and currently available small flexible ureteroscopes. Urology. 2003; 62: 218-22.
- Chew RH, Knudson BE, Deustedt JD: The use of stents in contemporary urology. Curr Opin Urol. 2004; 14: 111-5.
- Ramakumar S, Lancini V, Chan DY, Parsons JK, Kavoussi LR, Jarrett TW: Laparoscopic pyeloplasty with concomitant pyelolithotomy. J Urol. 2002; 167: 1378-80.
- Skrepetis K, Doumas K, Siafakas I, Lykourinas M: Laparoscopic versus open ureterolithotomy. A comparative study. Eur Urol. 2001; 40: 32-6.
- Goel A, Hemal AK: Upper and mid-ureteric stones: a prospective unrandomized comparison of retroperitoneoscopic and open ureterolithotomy. BJU Int. 2002; 89: 635-6.
_______________________
Received: October 6, 2004
Accepted after revision: January 13, 2005
_______________________
Correspondence address:
Dr. Rodrigo S. Quintela Soares
Rua Aluminio 50 / 31
Belo Horizonte, MG, 30220-090, Brazil
Phone: + 55 31 3222-2666
E-mail: quintelarod@yahoo.com