APPLIED
ANATOMIC STUDY OF TESTICULAR VEINS IN ADULT CADAVERS AND IN HUMAN FETUSES
(
Download pdf )
LUCIANO A. FAVORITO, WALDEMAR S. COSTA, FRANCISCO J.B. SAMPAIO
Urogenital Research Unit, State University of Rio de Janeiro, Rio de Janeiro, Brazil
ABSTRACT
Objectives:
Analyze the anatomic variations of the testicular veins in human cadavers
and fetuses.
Materials and Methods: One hundred male
adult cadavers and 24 fetuses were studied. Four anatomic aspects were
considered: 1) Number of testicular veins, 2) The local of vein termination,
3) Type and number of collaterals present and 4) Testicular vein termination
angle.
Results: Cadavers – Right side –
One testicular vein occurred in 85% and 2 veins in 5% of the cases. There
were communicating veins with the colon in 21% of the cases. Left side
– One testicular vein occurred in 82%, two veins in 15%, three veins
in 2% and four veins in 1% of the cases. There were communicating veins
with the colon in 31% of the cases. Fetuses – Right side –One
testicular vein occurred in all cases. This vein drained to the vena cava
in 83.3% of the cases, to the junction of the vena cava with the renal
vein in 12.5% and to the renal vein in 4.2%. There were communicating
veins with the colon in 25% of the cases. Left side – One testicular
vein occurred in 66.6% of the cases, and 2 veins in occurred 33.3%. Communicating
veins with the colon were found in 41.6% of the cases.
Conclusion: The testicular vein presents
numeric variations and also variations in its local of termination. In
approximately 30% of the cases, there are collaterals that communicate
the testicular vein with retroperitoneal veins. These anatomic findings
can help understanding the origin of varicocele and its recurrence after
surgical interventions.
Key
words: testis; spermatic cord; veins; varicocele; anatomy
Int Braz J Urol. 2007; 33: 176-80
INTRODUCTION
Varicocele
consists in the dilation of the pampiniform plexus veins, mainly on the
left side. It is a frequent pathology that occurs in approximately 15%
of male population, including children (1,2). Varicocele can be an important
cause of male infertility, and approximately 41% of infertile male patients
present varicocele (3).
Testicular venous drainage is done through
the pampiniform plexus, which in the region of the internal inguinal ring
gives origin to the testicular vein. The left testicular vein discharges
in the left renal vein in a straight angle, whereas the right testicular
vein discharges directly in the inferior vena cava in an oblique angle
(4). The testicular veins present valves in all its extension. In the
region of the fourth lumbar vertebra the testicular veins divided into
two trunks, one lateral and one medial (4,5). The lateral trunk is anastomosed
with retroperitoneal veins, mainly colonic and renal capsular veins, and
the medial trunk is anastomosed with ureteral veins. Anastomoses between
the two venous trunks are also found (4,5).
Studies on the anatomic distribution of
the testicular veins performed in cadavers are scarce (2,4). These studies
were done in fixed cadavers through the dissection of the retroperitoneum
with identification of the course of the gonadal vessels. There are no
studies in the indexed literature on the anatomy of the testicular veins
performed in human fetuses.
The objective of this work is to present
an analysis of the anatomical variations of number, local of drainage
and collaterals of the testicular veins, as well as of its distribution
in cadavers and in human fetuses.
MATERIALS AND METHODS
From
December 1998 to July 2006, 100 formalin-fixed cadavers and 24 fresh male
fetuses were studied. The cadavers were aged between 25 and 75 years and
did not present previous abdominal surgery. Identification of testicular
veins was performed through simple dissection. Four anatomic findings
were considered: 1) Number of testicular veins and the local of its division,
2) The local of the vein termination (inferior vena cava, renal vein or
angle between the renal vein and the inferior vena cava), 3) The type
and the number of collaterals (supra-renal, lumbar, accessory testicular)
and 4) The angle of testicular vein termination.
The fetuses studied were in excellent state
of conservation and ranged in age between 20 and 35 weeks post-conception
(WPC), calculated through the measurement of the largest feet (6-9). To
study the testicular veins in fetuses, a polyester microvascular resin
was injected through the intracardiac inferior vena cava, after a thoracotomy,
aiming to facilitate the identification and dissection of the testicular
veins, as described in previous papers (10). The same anatomic aspects
analyzed for the adults were considered for the fetuses.
RESULTS
Adult
Cadavers
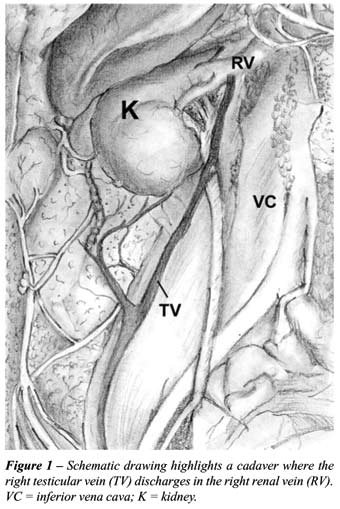
Right testicular vein – Of the 100
cases, we observed the presence of 1 testicular vein in 85% and of 2 veins
in 15%, totaling 115 testicular veins. The local of drainage of the testicular
vein when it has only one trunk was the inferior vein cava in 99 cases
and in 1 case the sole testicular vein drained to the right renal vein
(Figure-1). Among the 15 cases presenting 2 testicular veins, in 7 cases
the testicular vein ended in the angle between the renal vein and the
inferior vena cava. In 98% of the cases, the testicular vein drained in
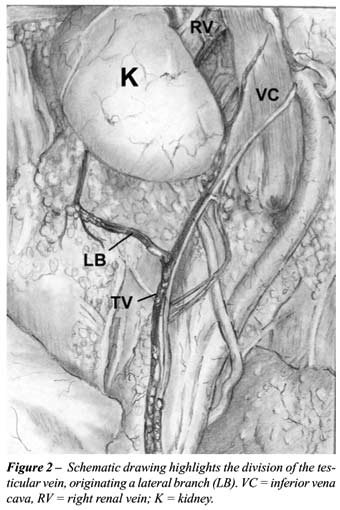
the vena cava in an acute angle, and in 1 case, the angle was straight.
In 21% of the cases, we observed collateral veins communicating with the
colon, which derived from the lateral division of the gonadal vein (Figure-2).
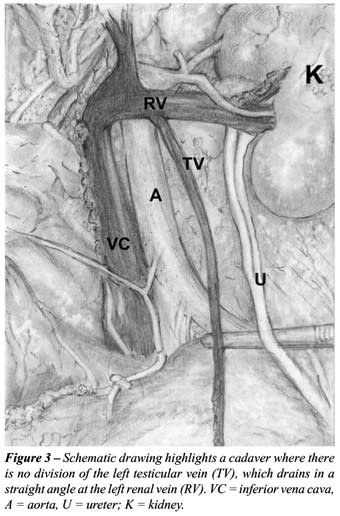
Left testicular vein – Of the 100
cases, we observed the presence of 1 testicular vein in 82% of the cases,
2 veins in 15% of the cases, 3 veins in 2% of the cases and 4 veins in
1% of the cases, totaling 122 testicular veins in the left side. The local
of drainage of the left side testicular veins was the renal vein in all
cases (Figure-3), independently of the number of testicular veins. The
angle of drainage of the left testicular vein in the renal vein was straight
in 95% of the cases. We observed the presence of veins communicating with
the colon, derived from the lateral division of the gonadal vein, in 31%
of the cases.
Fetuses
Right testicular vein – Of the 24
cases, we observed the presence of only 1 testicular vein in all cases.
The local of drainage of the testicular vein was in the inferior vena
cava in 83.3% of the cases, in the junction of the renal vein with the
inferior vena cava in 12.5%, and in the renal vein in 4.2% of the cases.
In 95.8% of the cases, the testicular vein drained in the vena cava with
an acute angle, and in 1 case, the angle was straight. The presence of
communicating veins with the colon, derived from the lateral division
of the gonadal vein, was found in 6 cases (25%).
Left testicular vein – Of the 24 cases,
we observed the presence of 1 testicular vein in 66.6% of the cases and
2 veins in 33.3% of the cases, totaling 32 left testicular veins. In all
cases, the local of drainage of the left testicular veins was the renal
vein. The left testicular vein drained in the renal vein with a straight
angle in 93.75% of the cases, and in 2 cases (6.25%), the angle was acute.
The presence of communicating veins with the colon, derived from the lateral
division of the gonadal vein, was found in 10 of the 24 fetuses (41.6%).
COMMENTS
Anatomic
variations of the testicular vein are frequent, especially concerning
the number of left side gonadal veins and the angle of termination of
these veins (4). These variations can be explained by the persistence
of primary venous systems that during the embryological period originate
the inferior vena cava (1,11). The left gonadal vein develops between
the 5th and the 7th weeks after conception, being derived from the distal
or post-renal portion of the sub-cardinal vein (12). In our sample, we
have observed the presence of variations in the number of testicular veins
of the right side in 15% of the cases in adult cadavers. In the left side,
we found the presence of multiple veins in 18% of the cases in adult cadavers
and in 33% of the case in fetuses, corroborating the high incidence of
numeric variation in the gonadal veins.
Anatomic variations of the local of drainage
of the testicular veins were found mainly at the right side. All left
testicular veins (either single of multiple) drained to the renal vein,
while the right testicular vein drained to the inferior vena cava in more
than 83% of the cases.
The treatment of varicocele can be performed
through various methods. This can be accomplished by open surgery, videolaparoscopic
surgery (13) or sclerotherapy (14). The objective of the treatment is
the obliteration of the veins that drain the testicle, while preserving
the vas deferens and the testicular artery (15). However, some studies
report that the ligature of the testicular artery together with the testicular
vein decreases the recurrence index after varicocele surgery, since there
are little veins close to the adventitia of the artery that can become
varicose after the exclusion of the main testicular vein, causing the
recurrence of the varicocele (16).
During performance of sclerotherapy, a contrast
medium is injected into the testicular veins, allowing the visualization
of the valves and the number and the course of the veins (1). Previous
studies have made evident that in approximately 74% of the cases, the
patients could present insufficiency in the valvar mechanisms of the gonadal
veins (1). In the present study, an analysis of the presence of valves
in the testicular vein was not accomplished.
In the past, the presence of collateral
branches of testicular veins was considered as anomaly, nevertheless,
a previous study with adults and neonates have found approximately 74%
of gonadal veins collaterals communicating with the colon (4). In our
sample, we found collaterals to the colon in 31% of the adult cadavers
and in 41% of the fetuses.
The incidence of recurrence after surgical
cure of varicocele varies from 0.6 to 45% (17), being the recurrence most
common after surgeries performed in pediatric patients (17). One of the
factors that seem to be involved in the recurrence after surgery of varicocele
is the anatomical distribution of the testicular veins in the retroperitoneum
(4). The presence of collateral veins communicating the testicular vein
with veins of the colon and with collateral veins at the opposite side,
could explain the compromise of spermatogenesis in cases of unilateral
varicocele, as well as the recurrence of varicocele after surgery (4).
The type of surgical technique could also favor recurrence. Retroperitoneal
ligature are the surgical procedure that course with the highest rates
of recurrence, between 10 and 15% (12). Microsurgical sub-inguinal ligature
is today the technique of choice for varicocele surgery, since this technique
is performed in a region that is closer to the testicle, decreasing the
chance of collaterals reactivation through retroperitoneal anastomoses.
CONCLUSIONS
Variations in the number and in the local of termination are frequent. In approximately 30% of the cases, there are collaterals that communicate testicular veins with retroperitoneal veins. These anatomical findings can help in understanding the origin of varicocele and its recurrence after surgical interventions.
ACKNOWLEDGMENT
Research supported by FAPERJ (Rio de Janeiro Foundation for Research Support) and CNPQ (National Council for Scientific and Technological Development), Brazil.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Braedel HU, Steffens J, Ziegler M, Polsky MS, Platt ML: A possible ontogenic etiology for idiopathic left varicocele. J Urol. 1994; 151: 62-6.
- Akbay E, Cayan S, Doruk E, Duce MN, Bozlu M: The prevalence of varicocele and varicocele-related testicular atrophy in Turkish children and adolescents. BJU Int. 2000; 86: 490-3.
- Beck EM, Schlegel PN, Goldstein M: Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol. 1992; 148: 1190-4.
- Wishahi MM: Detailed anatomy of the internal spermatic vein and the ovarian vein. Human cadaver study and operative spermatic venography: clinical aspects. J Urol. 1991; 145: 780-4.
- Sofikitis N, Dritsas K, Miyagawa I, Koutselinis A: Anatomical characteristics of the left testicular venous system in man. Arch Androl. 1993; 30: 79-85.
- Hern WM: Correlation of fetal age and measurements between 10 and 26 weeks of gestation. Obstet Gynecol. 1984; 63: 26-32.
- Mercer BM, Sklar S, Shariatmadar A, Gillieson MS, D’Alton ME: Fetal foot length as a predictor of gestational age. Am J Obstet Gynecol. 1987; 156: 350-5.
- Platt LD, Medearis AL, DeVore GR, Horenstein JM, Carlson DE, Brar HS: Fetal foot length: relationship to menstrual age and fetal measurements in the second trimester. Obstet Gynecol. 1988; 71: 526-31.
- Streeter GL: Weight, sitting. height, head size, foot length, and. menstrual age of the human embryo. Contrib Embryol Carnegie Inst. 1920; 11:143-70.
- Sampaio FJ, Favorito LA, Freitas MA, Damiao R, Gouveia E: Arterial supply of the human fetal testis during its migration. J Urol. 1999; 161: 1603-5.
- Itoh M, Moriyama H, Tokunaga Y, Miyamoto K, Nagata W, Satriotomo I, et al.: Embryological consideration of drainage of the left testicular vein into the ipsilateral renal vein: analysis of cases of a double inferior vena cava. Int J Androl. 2001; 24: 142-52.
- Forte F, Latini M, Foti N, Sorrenti S, De Antoni E, Virgili G, et al.: Bahren types III and IVa testicular vein anomalies as a reason for failure in left idiopathic varicocele retrograde sclerotherapy. Ontogenic discussion and clinical implications. Surg Radiol Anat. 2001; 23: 427-31.
- Nagler HM, Luntz RK, Martinis FG: Varicocele. In Lipshultz LI, Howars SS (eds.), Infertility in the male. Third edition. St.Louis, Mosbi Year Book. 1997.
- Tauber R, Johnsen N: Antegrade scrotal sclerotherapy for the treatment of varicocele: technique and late results. J Urol. 1994; 151: 386-90.
- Pryor JL, Howards SS: Varicocele. Urol Clin North Am. 1987; 14: 499-513.
- Matsuda T, Horii Y, Yoshida O: Should the testicular artery be preserved at varicocelectomy? J Urol. 1993; 149: 1357-60.
- Goldstein M: Complications and results of varicocelectomy. In: Surgery of male infertility. Phyladelphia, WB Saunders Company. 1995; pp. 194-6.
____________________
Accepted after revision:
October 23, 2006
_____________________
Correspondence address:
Dr. Luciano A. Favorito
Urogenital Research Unit - UERJ
Av. 28 de Setembro, 87 – fundos – FCM – terreo
20551-030, Rio de Janeiro, RJ, Brazil
Fax: + 55 21 2587-6121
E-mail: lufavorito@yahoo.com.br