SURGICAL
TECHNIQUE USING ADVANCETM SLING PLACEMENT IN THE TREATMENT OF POST-PROSTATECTOMY
URINARY INCONTINENCE
(
Download pdf )
DAVID E. RAPP, W. STUART REYNOLDS, ALVARO LUCIONI, GREGORY T. BALES
Section of Urology, Department of Surgery, University of Chicago Pritzker School of Medicine, Chicago, Illinois, USA
ABSTRACT
Objectives:
To describe and illustrate a new minimally invasive approach to the treatment
of male stress urinary incontinence following prostatectomy.
Surgical Technique: Our initial experience
consisted of four patients treated with the Advance sling for post-prostatectomy
urinary incontinence. Sling placement involves the following steps: 1.
Urethral dissection and mobilization, 2. Identification of surgical landmarks,
3. Placement of needle passers through the obturator foramen, 4. Mesh
advancement, 5. Mesh tensioning and fixation, 6. Incision closure.
Comments: Based on our initial experience,
we believe that the Advance Male Sling System may be a safe technique
for the treatment of male stress urinary incontinence. This technique
is easy to perform and may offer a reproducible, transobturator approach.
Further patient accrual is ongoing to assess the safety and reproducibility
of this technique. Also, additional study will focus on efficacy standards
and complication rates.
Key
words: prostatectomy; urinary incontinence; stress; prostheses
and implants; suburethral slings
Int Braz J Urol. 2007; 33: 231-7
INTRODUCTION
The
rate of post-prostatectomy incontinence (PPI) ranges between 3 and 60%
(1). The treatment of PPI is often difficult and many patients ultimately
require surgical intervention for symptom alleviation. Although the artificial
urinary sphincter (AUS) remains the standard for post-prostatectomy incontinence
surgery, it has several limitations. Foremost, the AUS can be associated
with infection or the need for revision and is costly (1). Alternative
techniques include bulking agent injection (collagen, Coaptite®, Macroplastique®),
balloon urethral compression devices (ProAct®), and the male urethral
sling.
The male sling has been reported in the
literature with increasing frequency, and several different techniques
have been described (2-4). Although encouraging results have been reported
by many using the male sling, the variety in technique and lack of long-term
outcomes have limited the widespread use of this surgical option. Further,
outcome variability remains problematic (2).
The AMS AdVance Male Sling is a new mesh
system developed for the treatment of male stress urinary incontinence.
This system is provided in a single kit and is deployed in a transobturator
approach using a trochar system similar to mesh systems widely used in
the treatment of female stress urinary incontinence. Accordingly, surgeon
familiarity and procedure reproducibility may be optimized. The aim of
this report is to describe the surgical technique for repair of post-prostatectomy
incontinence using the AdVance system.
SURGICAL TECHNIQUE
The AMS AdVance Male Sling is a polypropylene mesh system developed for the treatment of male stress urinary incontinence. Our initial experience consisted of patients treated with the Advance sling for post-prostatectomy urinary incontinence. Men were selected based on the presence of documented stress incontinence. Per study protocol, all patients are evaluated in the office with a full history, physical examination, and urinalysis. One hour and 24-hour pad tests are performed. Subjective evaluation includes completion of the three following questionnaires: the International Consultation of Incontinence (ICI) questionnaire, the Incontinence Quality of Life (IQOL) questionnaire, and the UCLA/RAND questionnaire. All patients subsequently undergo cystoscopy to rule out the presence of stricture or other defined etiology of urinary incontinence. Finally, all patients undergo complete urodynamic evaluation.
AMS
Advance Male Sling System Description
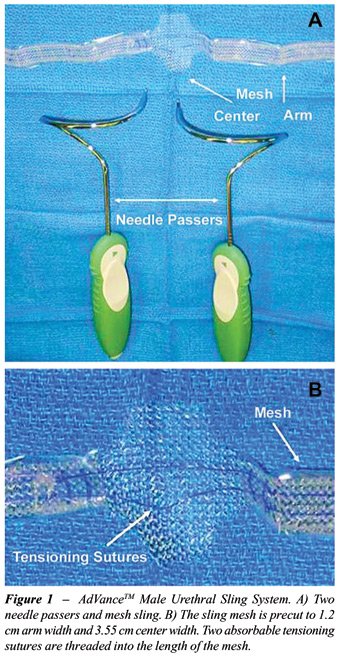
The AMS Advance Male Sling System is comprised
of two needle passers and a mesh sling (Figure-1A). The sling mesh is
constructed of polypropylene monofilament mesh that is precut to 1.2 cm
arm width and 3.55 cm center width. Two absorbable tensioning sutures
are threaded into the length of the mesh to spread fixate the mesh, allowing
for flat coaptation of the urethra (Figure-1B). Further, these tensioning
sutures allow for maintenance of mesh tension following placement. Plastic
sheaths are placed over the mesh arms to provide ease in placement.
Surgical
Technique
Appropriate anesthesia is established using
general anesthesia; however, spinal anesthetic may also be used. Patients
are positioned in the extended dorsal lithotomy position. A 16F Foley
catheter is placed to drain the bladder. Peri-operative antibiotics are
administered, comprising Ampicillin and Gentamicin, preferred in our experience
for cases involving foreign body insertion.
A vertical incision is made to the perineum
approximately 1-2 cm inferior to the penoscrotal junction and carried
1 cm anterior to the rectum. Dissection is continued through Colles’
fascia and the underlying bulbocavernous muscle. Sharp dissection is continued
until the spongiosal bulb has been freely dissected. The perineal body
is identified and dissection is continued proximally approximately 4 cm.
Attention is then focused on identification
and marking of the anatomical landmarks for placement of the surgical
passers. Initially, the adductor longus tendon is identified and marked
(Figure-2, solid arrow). Each of the two trochar insertion sites are then
marked, such that insertion is performed just lateral to the inferior
pubic ramus (Figure-2, broken arrow). The insertion site is generally
2 cm below the adductor longus tendon such that insertion is performed
at a point one third below the cephalad peak of the obturator foramen.
Accordingly, a 45º angle between insertion and exit sites (at the
level of the perineal body) is maintained.

Following marking, the skin sites are incised
and surgical passer placement is begun. The surgeon’s finger is
placed inside the perineal dissection and again identifies the inferior
pubic ramus where the passer will exit. Under manual guidance, the passer
is advanced through the medial aspect of the obturator foramen, exiting
at the level of the perineal body lateral to the spongiosal bulb (Figure-3).
Care is taken to maintain a 45º angle during passage, which is aided
by keeping the surgeon’s hand close to the buttock and completing
the trochar rotation. The passer is then hooked to the respective sling
arm, which are then pulled though the obturator foramen to exit via the
skin incision. This maneuver brings the mesh in place. The mesh is checked
at this point to ensure that twisting has not occurred. Subsequently,
the opposite passer is placed in a similar manner and the sling is pulled
into place.

Attention is now focused on sling positioning
and tension. The central mesh anchor is sutured into place, with the posterior
aspect fixed to the spongiosal tissue at the most proximal aspect of the
bulbar dissection. The distal anchor is then sutured to the spongiosal
tissue, each performed with 3-0 vicryl suture (Figure-4A). Tensioning
of the sling is now performed, by pulling the mesh arms such that the
bulb of the corpus spongiosum is brought cephalad by the sling. Sling
tensioning in increased until 3-4 cm of proximal urethral movement is
obtained. Bulbar suspension is confirmed by measuring proximal movement
from the initial point of fixation to the perineal body (Figure-4B). Cystourethroscopy
is performed to rule out urethral or bladder injury. The arms of the mesh
are cut below skin level and skin incisions closed with Dermabond (Ethicon,
Somerville, NJ). The perineal dissection is then closed with a standard
3-layer closure with absorbable suture.

In our experience, patients may be discharged
home immediately after surgery or admitted for overnight observation.
The Foley catheter is maintained overnight. Patients discharged home following
surgery are given instructions enabling them to remove the catheter at
home. All patients receive five days of appropriate oral antibiotic coverage.
Surgical
Experience
Since August 2006, a total of 4 patients
have undergone AdVance sling placement. The mean patient age was 62 years.
Mean 1-hour and 24-hour pad test weight were 5.3 and 38 grams, respectively.
Average daily pad use was 3 pads/day. Stress incontinence was confirmed
with urodynamic evaluation is all patients. Mean Valsalva leak point pressure
was 101 cm H2O. Mean pre-operative IQOL-SF score was 16.
Mean estimated blood loss was 142 mL and
mean surgical time was 97 minutes. Significant urethral coaptation following
sling placement was confirmed using cystourethroscopy in all patients.
There were no intra-operative complications. All patient but one underwent
Advance placement as an outpatient procedure, with the remaining patient
being discharged home the following morning. All Foley catheters were
removed the morning of POD one.
COMMENTS
The
use of fixed urethral compression for the treatment of male stress urinary
incontinence has been reported over the last four decades. The modern
era of fixed urethral compression procedures has been marked primarily
by the male urethral sling. Although various sling procedures exist, two
general techniques have been reported with greatest frequency. In the
first, periurethral compression bolsters are anchored over the rectus
fascia via a separate abdominal incision (3). Alternatively, the use of
bone screws to secure a periurethral mesh has been described in order
to avoid a separate abdominal incision (2,4).
Short-term outcomes using these techniques
have been favorable. However, result variability may exist based on surgeon,
technique used, and definition of success (2,4). Certainly, the variation
of reported results raises concerns about the reproducibility of these
procedures. A second concern specific to the latter technique surrounds
the placement of bone anchors, which may be associated with osseous complications
such as infection or pain (4).
Concurrently, a greater experience has been
reported using both the transobturator approach and mesh synthetics in
the treatment of female stress urinary incontinence. Accordingly, multiple
experiences demonstrate that midurethral sling placement using the transobturator
approach is associated with excellent success rates and minimal complications
(5). In addition, the use of synthetic mesh has gained greater popularity
owing to its availability, consistent quality, inert properties, and low
cost. The use of synthetic mesh has also been associated with an improved
success rate in perineal male sling experience when compared to absorbable
materials (e.g. dermis, fascia lata, SIS) (2).
We believe that the transobturator male
sling placement represents an evolution in the treatment of male stress
urinary incontinence. Foremost, this procedure restores physiologic voiding
in a minimally invasive fashion using mesh, and is less expensive when
compared to the AUS. The AdVance is placed via a transobturator approach,
which has become popularized in the placement of midurethral slings, owing
to its ease, reproducibility, and low rate of complications. Accordingly,
surgeon familiarity is high, which may improve procedure reproducibility
when compared to the variety of alternative male sling procedures. In
addition, this approach allows for avoidance of bone anchors and related
issues.
CONCLUSIONS
Based on our initial experience, we believe that the Advance Male Sling System may be a safe technique for the treatment of male stress urinary incontinence. This technique is easy to perform and may offer a reproducible, transobturator approach. Further patient accrual is ongoing to assess the safety and reproducibility of this technique. Also, additional study will focus on efficacy standards and complication rates.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Migliari R, Pistolesi D, Leone P, Viola D, Trovarelli S: Male bulbourethral sling after radical prostatectomy: intermediate outcomes at 2 to 4-year followup. J Urol. 2006; 176: 2114-8.
- Onur R, Rajpurkar A, Singla A: New perineal bone-anchored male sling: lessons learned.Onur R, Rajpurkar A, Singla A. Urology. 2004; 64: 58-61.
- Stern JA, Clemens JQ, Tiplitsky SI, Matschke HM, Jain PM, Schaeffer AJ: Long-term results of the bulbourethral sling procedure. J Urol. 2005; 173: 1654-6.
- Madjar S, Jacoby K, Giberti C, Wald M, Halachmi S, Issaq E, et al.: Bone anchored sling for the treatment of post-prostatectomy incontinence. J Urol. 2001; 165: 72-6.
- Waltregny D, Reul O, Mathantu B, Gaspar Y, Bonnet P, de Leval J: Inside out transobturator vaginal tape for the treatment of female stress urinary incontinence: interim results of a prospective study after a 1-year minimum followup. J Urol. 2006; 175: 2191-5.
____________________
Accepted after revision:
December 14, 2006
_______________________
Correspondence
address:
Dr. David E. Rapp
Section of Urology
Univ Chicago Pritzker School of Medicine
MC 6038, 5841 S. Maryland Ave.
Chicago, IL 60637, USA
E-mail: derapp@yahoo.com
EDITORIAL COMMENT
Post-prostatectomy
urinary incontinence is a problem for which there is currently no satisfactory
treatment. Although the artificial urinary sphincter is considered the
gold standard treatment, it is an expensive and complicated procedure,
which is not exempt of short-, medium- and long-term risks.
The author describes the experience of patients
treated for post-prostatectomy urinary incontinence using the AdVanceTM
Male Sling system. The main steps required for the correct use of this
technique following the transobturator approach are described in detail,
as an alternative to the bulking agent injection and the male urethral
sling approaches. At this point, it is worth mentioning that there are
other alternative treatments for male incontinence such as the implant
of a silicone balloon (ProACT), the use of an adjustable external mechanical
regulator (ReMeEx) and specially the implantation of an adjustable bulbourethral
sling (Argus). In this matter, we would like to comment that as opposed
to female incontinence, the treatment of post-prostatectomy male urinary
incontinence must pursue to obtain maximum tension and we doubt this is
achieved using the trasobturator approach as effectively as adjustable
and regulatable systems.
It would be advisable that the author clarifies
the number of patients he has treated and his experience with respect
to initial results even if these were only short term.
However, his description of the technique
and visual aids are outstanding and we encourage the author to continue
carry on his hard work and to publish his results as soon as possible.
Dr.
Jesús Moreno Sierra
Department of Urology
Hospital Clinico San Carlos
Complutense University
Madrid, Spain
E-mail: dr_jmoreno@hotmail.com
The
worldwide experience with the use of suburethral slings for the treatment
of post-radical prostatectomy stress urinary incontinence is growing,
and clearly showing its efficacy and reproducibility, also on the long
run (1,2). The different surgical techniques employed may vary on the
“scaffold” used to secure the sling, either the rectus fascia
or the pubic rami (3, 4). However, share the concept of suspension and
compression they ensure to the bulbar urethra, allowing physiological
voiding, taking into account changes in abdominal pressure and impaired
manual dexterity, which could be, on the other hand, an important issue
when the artificial urinary sphincter is considered (5).
The
article published in the present issue of the International Braz J Urol
by Rapp and co-workers is quite interesting as it seems to show promise
that good results can be also achieved passing and fixing the sling through
the obturator foramen, as other authors have already shown (6). Although
the number of patients studied is still too low and no follow-up is provided
yet, this approach must be viewed with great interest because of the transobturator
approach used, which could definitely become the standard one, for its
ease, reproducibility and low complications rate, provided it will stand
the proof of time.
REFERENCES
- Stern JA, Clemens JQ, Tiplitski SI, Matschke HM, Jain PM, Schaeffer AJ: Long-term results of the bulbourethral sling procedure. J Urol. 2005; 173: 1654-6.
- Migliari R, Pistolesi D, Leone P, Viola D, Trovarelli S: Male bulbourethral sling after radical prostatectomy: intermediate outcomes at 2 to 4-year followup. J Urol. 2006; 176: 2114-8.
- Schaeffer AJ, Clemens JQ, Ferrari M, Stamey TA: The male bulbourethral sling procedure for post-radical prostatectomy incontinence. J Urol. 1998; 159: 1510-5.
- Madjar S, Jacoby K, Giberti C, Wald M, Halachmi S, Issaq E, et al.: Bone anchored sling for the treatment of post-prostatectomy incontinence. J Urol. 2001; 165: 72-6.
- Raz S, Gousse AE: The male bulbourethral sling procedure for post-radical prostatectomy incontinence: editorial comment. J Urol. 1998; 159: 1515-6.
- Palma PC, Dambros M, Thiel M, Romano V, Griguol O, Ricetto CL, et al.: Readjustable transobturator sling: a novel sling procedure for male urinary incontinence. Urol Int. 2004; 73: 354-6.
Dr. Domenico Viola
Dr. Sergio Leoni
U.O.C. Urologia
Arcispedale Santa Maria Nuova
Azienda Ospedaliera di Reggio Emilia
Reggio Emilia, Italy
E-mail: domenico.viola@asmn.re.it