SPONTANEOUS
RESOLUTION RATES OF VESICOURETERAL REFLUX IN BRAZILIAN CHILDREN: A 30-YEAR
EXPERIENCE
(
Download pdf )
MIGUEL ZERATI FILHO, ADRIANO A. CALADO, UBIRAJARA BARROSO JR, JOAO L. AMARO
Division of Urology, Sao Paulo State University, UNESP, Botucatu, Sao Paulo, Brazil
ABSTRACT
Objective:
We evaluated clinical characteristics of primary vesicoureteral reflux
(VUR) in infants in a 30-year period in Brazil with special reference
to the relation of renal parenchymal damage to urinary tract infection
and gender.
Materials and Methods: From 1975 through
2005, 417 girls (81.6%) and 94 boys (18.4%) with all grades of reflux
were retrospectively reviewed. Patients were categorized by the worst
grade of reflux, maintained on antibiotic prophylaxis and underwent yearly
voiding cystourethrography until the reflux was resolved. VUR was considered
resolved when a follow-up cystogram demonstrated no reflux. Surgical correction
was recommended for those who fail medical therapy, severe renal scarring
or persistent VUR.
Results: Grades I to V VUR resolved in 87.5%,
77.6%, 52.8%, 12.2% and 4.3%, respectively. Renal scars were present at
presentation in 98 patients (19.2%). Neither gender nor bilaterality versus
unilaterality was a helpful predictor of resolution. The significant difference
was found among the curves using the log rank (p < 0.001) or Wilcoxon
(p < 0.001) test.
Conclusion: Despite the current use of screening
prenatal ultrasound, many infants are still diagnosed as having vesicoureteral
reflux only after the occurrence of urinary tract infection in our country.
Scarring may be associated to any reflux grade and it may be initially
diagnosed at any age but half of the scars are noted with higher grades
of reflux (IV and V). The incidence of reflux related morbidity in children
has significantly diminished over the last three decades.
Key
words: ureter; vesico-ureteral reflux; reconstructive surgical
procedures
Int Braz J Urol. 2007; 33: 204-15
INTRODUCTION
Vesicoureteral
reflux (VUR) is a common pediatric problem. The possibility of renal damage
due to VUR and consequently renal function impairment and hypertension
gives the necessary impetus for the diagnosis or exclusion of this problem
(1). In general, it was thought that medical and surgical management represented
equally efficacious treatment options (1,2). Both treatment forms have
advantages and disadvantages that must be taken into account and shared
with the parents when choosing the best approach. If, on one hand, clinical
treatment requires chronic antibiotic prophylaxis, periodic surveillance
of urine cultures and periodic voiding cystourethrograms (VCUGs), which
despite the low morbidity may cause discomfort, on the other hand, surgery
is related to the risks of a surgical-anesthetic procedure.
Several studies carried out in Europe and
in the United States have established the rates of spontaneous resolution
for patients with VUR undergoing medical management. Due to the lack of
similar data in our country, specialists have used these data for management
of the patients.
The primary endpoint of this study was defining
the rates of spontaneous resolution for patients with VUR in our country.
These data may be helpful to determine the need for surgical intervention
and the proper follow-up schedule in patients on antibiotic prophylaxis.
On the other hand, the group selected in
this report, which was conservatively managed over a 30-year period, is
of particular interest in understanding the changes in the approach of
VUR in this period of time. Besides finding out the overall resolution
rate, we saw if we could find differences between the groups according
to the period diagnosis was carried out.
MATERIALS AND METHODS
Of
the 813 consecutive patients with VUR treated at our institution from
January 1975 to December 2005, 302 were excluded because in 121 a VCUG
was not repeated, in 105 follow-up were insufficient (< 12 months)
and 76 children had secondary VUR. 511 children were retrospectively evaluated
and met the inclusion criteria: a) age < 10 years at the time of diagnosis;
b) radiological tests confirming VUR and VUR grade; c) minimum follow-up
time of 12 months; d) no voiding dysfunction, neuropathic bladder, duplicated
systems, ectopic ureters, ureterocele, and other associated pathologies.
VUR was detected by VCUG and the grade classified according to the International
Reflux Study Committee (3).
The renal parenchyma was evaluated using
renal cortical scintigraphy (99mTc-DMSA), intravenous urography
or both (4-6). Patients were kept under continuous prophylaxis and had
urine culture collected on a monthly basis, upper urinary tract assessment
with renal ultrasonography (RUS) every six months and intravenous urography
or scintigraphy and VCUG once a year. Reflux was considered resolved when
absent on a single cystogram.
Patients with any of the following parameters
underwent surgery: failure of medical management (breakthrough urinary
tract infections and patient noncompliance), increase or development of
new renal scars and reflux that fails to resolve (mainly grade IV or V).
After obtaining demographic data, patients
were divided into three groups according to the period diagnosis was carried
out: Group A (n = 80) from 1975 to 1985; Group B (n = 205) from 1986 to
1995; Group C (n = 226) from 1996 to 2005.
The results were statistically analyzed
using the Minitab® statistical computing software, with p < 0.05
considered to indicate statistical significance. Kaplan-Meier curves were
constructed to estimate the reflux resolution rate per grade and the rates
were compared using the log rank and Wilcox on tests. Data shown in the
tables were analyzed by the chi-square test. The study protocol was reviewed
and approved by the local ethics committee.
RESULTS
The
initial clinical manifestation leading to the diagnosis of VUR in 85%
of the cases was urinary tract infection, confirmed by urinary culture,
followed by fever of indeterminate cause (5.4%), lumbar pain (3.5%), antenatal
hydronephrosis (2.9%), hematuria (2.5%) and others. Mean age at presentation
was 3.1 years and median follow-up was 2.7 years (1.2 - 12.4 years). VUR
was unilateral in 250 (48.9%) and bilateral in 261 (51.1%) cases. Grade
II VUR was detected more frequently (192 cases – 37.6%), followed
by grade III (174 cases - 34%), grade IV (74 cases – 14.5%), grade
I (48 cases – 9.4%) and grade V (23 cases – 4.5%).
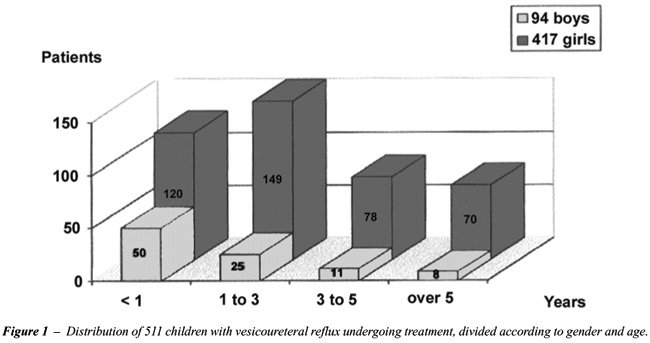
We observed an incidence 4 times greater
in females than in males (81.6% against 18.4%). When patients were stratified
according to age at diagnosis, it was observed that the number of boys
with VUR decreases with age, ranging from 29.4% in the first year of life
to 10.2% in children over 5 years of age. One hundred and twenty female
patients (70.6%) had a diagnosis of VUR before 1 year of age, whereas
89.8% (70/78) girls had a diagnosis of VUR over 5 years of age.
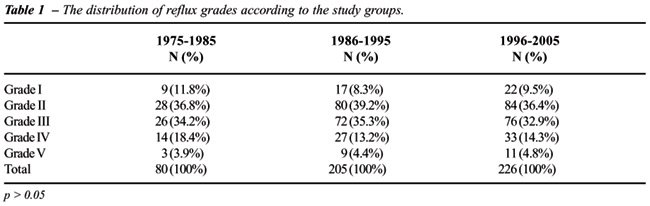
The large majority of diagnosis, 344 (67.3%),
was made before the 3rd year of life, of which 170 (33.2%) before the
first year (Figure-1). The stratification of patients according to VUR
grade shows a similar distribution among the three groups (Table-1). There
was no significant difference among the study groups (A, B and C) for
the severity of VUR. Table-2 shows the tests carried out in the initial
evaluation of the patients in the study groups. For the statistical analysis,
groups A and B were analyzed together due to the small sample of patients
who carried out RUS and DMSA scan in group A. In the first period, intravenous
urography was carried out in 93.7% of the cases and RUS and DMSA scan
in 1.2% and 13.7% respectively. In the last decade there is an important
change, and intravenous urography is used in only 21.2% of the children
and RUS and scintigraphy is used in 88% and 23.4% respectively. There
is a significant difference between groups (A+B) and C for the use of
RUS, scintigraphy and intravenous urography (p < 0.001).
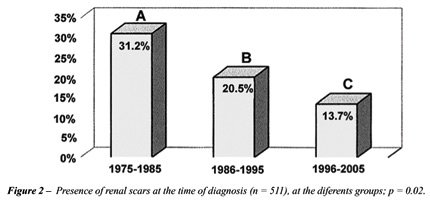
Patients were also evaluated for the presence
of renal scars at the time of diagnosis. In group A, 31.2% (25/80) had
renal scars, in group B, 20.5% (42/205); and in group C, 13.7% (31/226)
(Figure-2). There was a significant difference between groups for the
presence of renal scars in the initial evaluation (p = 0.02), with a clear
decrease of renal scars in the last period, from 1996 to 2005. Table-3
stratifies patients with renal scars according to age at the presentation.
There is a clear correlation between age and renal scars, which are significantly
more frequent in the group of patients over 5 years of age (p < 0.001).
Of the 125 patients requiring surgery, 30%
(24/80) were from Group A, 30.2% (62/205) from Group B and 17.2% (39/226)
from Group C. When the number of surgical procedures is compared, a significant
difference is observed between Groups A and B compared to Group C (p =
0.003), with a clear decrease of surgical indications over time. In the
overall characteristics of patients (Table-4), severe cases of reflux
(IV and V) are observed in 19% of the children and the incidence of renal
injury is proportional do VUR grade, i.e., the more intensive the VUR,
the greater is the probability of developing scars. However, even low
grade VUR (I and II) was associated with renal scarring in this cohort.
When the rates of spontaneous resolution
of reflux were analyzed for different grades of VUR throughout the medical
management, 87.5% (42/48) of the patients with VUR grade I; 77.6% (149/192)
of patients with VUR grade II and 52.8% (92/174) of patients with VUR
grade III had spontaneous resolution (Figure-3). Of the 74 patients with
VUR grade IV, spontaneous resolution was observed in 9 (12.2%) patients.
Only 1 patient with VUR grade V had spontaneous resolution during follow-up.
There is no significant difference of spontaneous
resolution with clinical treatment when boys and girls are compared. The
resolution of VUR was not affected by age at entry. As to the laterality
of VUR, there was no significant difference of cure for unilateral or
bilateral VUR for grades I, II and III (p = 0.731; p = 0.344; p = 0.204,
respectively). However, for patients with VUR grade IV, there was spontaneous
resolution in 8 patients with unilateral (19%) disease and in only 1 case
of bilateral VUR (3.1%) (p = 0.068).
The analysis of Kaplan-Meier curves (Figure-3)
showed a significant difference (p < 0.0001). Table-5 shows the probability
of spontaneous cure of VUR at 2 and 5 years of follow-up based on a transversal
section of the Kaplan-Meier curves.

COMMENTS
Despite
the large number of children with reflux, management among urologists
is still controversial. One of the most debated aspects is the choice
between observation or surgical treatment. Although there is no consensus
for the treatment of VUR in childhood, several principles based on literature
data and corroborated by this study may be used as parameters when choosing
optimal therapy for each case.
Chronic reflux nephropathy is a well known
and feared disease and is the cause of chronic renal failure in up to
25% of children undergoing dialysis and in 10 to 15% of adults waiting
for renal transplantation (7).
Several factors are taken into consideration
when choosing therapy for VUR, such as: age, VUR grade, presence of renal
injury, history of urinary infections and tolerance to antibiotics. The
prevention of irreversible renal injury is the final goal of any of the
therapeutic modalities, and so far there is no evidence of the superiority
of clinical treatment over surgical therapy (8).
Wheeler et al. (8) recently perform a meta-analysis
of seven trials with 833 evaluated patients comparing antibiotic prophylaxis
with combined surgery and antibiotics to obtain summary measures of treatment
effects. This systematic review of randomized controlled trials of interventions
for children with vesicoureteral reflux has identified a number of important
and unanswered questions. Most importantly, it is not clear whether any
intervention for children with primary vesicoureteral reflux does more
good than harm. Assuming intervention is beneficial, it is not clear whether
antibiotics alone or reimplantation surgery alone are most effective in
reducing the risk of urinary tract infection and renal parenchymal abnormality.
Furthermore, the trials, which have been undertaken comparing surgery
and antibiotics with antibiotics alone, have not shown any additional
benefit of surgery except for a reduction in risk of febrile urinary tract
infections.
Because of the good results obtained with
clinical therapy using low dose antibiotics, in addition to the fact that
there are few prospective, randomized, studies comparing clinical treatment
to surgery (9-11), the large majority of children with VUR is clinically
treated. Thus, high rates of spontaneous resolution are obtained, which
depend especially on VUR grade and age at the time of diagnosis.
The most frequent clinical abnormality leading
to the diagnosis of VUR is UTI. In our series, 85% of the children had
UTI as an early manifestation. Recent studies have shown that other causes,
such as antenatal hydronephrosis and voiding dysfunction have played a
larger role in the diagnosis of VUR (12). In the evaluation of International
Reflux Study in Children (IRSC) (10), UTI was observed in 89% to 92% of
children with VUR, and in approximately 30% of the cases there was some
degree of renal injury at the time of diagnosis.
Of the 511 patients in this study, 98 (19.2%)
had renal scars at the time of diagnosis, and scarring was significantly
more frequent in patients with VUR grades IV and V (48.6% and 87% respectively).
Greenfield et al. (12), in a study with 1040 children, diagnosed renal
scarring in 13% of the cases, of which 22% did not have a prior history
of UTI. The stratification of patients in three different periods of time
according to the time of diagnosis (Groups A, B and C) allowed us to carry
out a critical analysis of the long-term outcome of VUR therapy. As occurs
in IRSC (10), most children in the first period of our study (98.7%) underwent
intravenous urography for the assessment of the upper urinary tract, and
this method was replaced by RUS and DMSA scan in the subsequent periods.
There was a clear change in the renal assessment of patients with VUR.
The incidence of renal scarring at the time
of VUR diagnosis was 31.2% in the first period (Group A) against 13.7%
in the last group (Group C). A probable explanation for the high incidence
of renal scars in the first period (group A) is a combination of many
factors. First of all in the 1970s and early 1980s It was not a common
practice for infants following their first diagnosed UTI to be referred
to routine diagnostic imaging and we know that The likelihood of developing
renal scars depends on factors such as the number of symptomatic UTI and
the delay in their treatment. Actually the importance of prompt treatment
of urinary infection or symptomatic recurrence of UTI was emphasized to
local physicians. A second explanation is that patients admitted until
the end of the 80’s had a greater risk of UTI than children with
a diagnosis of VUR after 1990. Possibly, this fact reflects an improvement
in our understanding of the risk factors for UTI in this population, especially
the recognition and treatment of voiding dysfunction and constipation.
In 24.5% (125/511) of the cases, surgical
procedures were carried out to repair VUR. Skoog et al. (13) and Greenfield
et al. (12), using similar indication criteria, reported 14% to 20% of
surgical treatment. The surgical indications decreased from 30%, in the
first period, to 17.2% in the last, following the currently used criteria.
This decrease is probably related to a better understanding of the disease
and more adequate follow-up of these children. Despite the excellent success
rates following antireflux surgery one has to bear in mind that surgery
only corrects the anatomical abnormality. The long-term outcome with regard
to renal function, urinary tract infections and arterial hypertension
does not differ significantly from the medication group.
In our study, the Kaplan-Meier curves of
VUR resolution show a clear relationship between the possibility of cure
and the follow-up time, showing that VUR grades I and II were cured significantly
faster than grades III and IV. Other authors (8,14) have mentioned similar
results. The information regarding the probability of resolution is essential
when passing information onto the parents and choosing the best therapy
to be adopted. Our spontaneous cure results are in agreement with those
of other studies (15,16). Schawab et al. (8) have reported 83% and 76%
of spontaneous regression for grades I and II respectively. Tamminen-Mobius
et al. (17) obtained resolution in 63% of VUR grade II and 50% in grade
III. In our casuistic we obtained 87.5% of spontaneous cure for grade
I, 77.6% for grade II and 52.8% for grade III, when the follow-up period
is taken into consideration. The spontaneous resolution of VUR grade IV
with clinical therapy is known to be low. In our study, the expected probability
of cure at 5 years is only 12.2%. Results have shown a spontaneous cure
ranging from 9 to 16% in patients with VUR grade IV (13,16).
The well-known association between vesicoureteral
reflux and urinary tract infection is the basis for pathophysiological
and therapeutic implications, which have dominated the literature on the
subject for the last 3 decades. The pathogenesis of renal damage in children
with VUR is controversial, as the exact role of UTI and pressure effects
of sterile reflux on the developing kidneys is still unknown.
Primary VUR diagnosed after prenatal hydronephrosis
is usually severe and is often associated to a congenital renal scars,
which is primary and not the result of UTI. In our study diagnosis of
VUR resulting from antenatal hydronephrosis were observed only in 15 (3%)
children. This type of VUR affects male more than female infants and the
male predominance is thought to be secondary to a transient infravesical
obstruction during pregnancy. This specific group of children achieves
up to 43% of spontaneous cure for grades IV and V (18-20). Although in
the first type of reflux renal scarring is often present at diagnosis,
then probably congenital, it may always progress after UTI; hence the
importance of early diagnosis and careful follow-up in each infant with
primary VUR.
Our results showed that the incidence of
reflux-related morbidity in children has significantly diminished over
the last three decades. In our country, the rates of reflux-related nephropathy
are much less than reported historically and are consistent with the most
recently reported international data.
In our experience, and based on current
knowledge and guidelines, which derive from a thorough review of the literature
the recommendation of a treatment strategy for VUR is not, however, straightforward.
In deciding whether to recommend surgical correction of VUR, factors that
should be considered to include the previous and potential future morbidity
of VUR in that individual, the risk of uncorrected VUR, the likelihood
of spontaneous resolution or significant reduction in VUR, the efficacy
and complications of medical therapy, the morbidity and discomfort associated
to serial screening for VUR, the benefits and risks of surgical therapy,
and economic factors.
The probability of spontaneous resolution
of VUR forms the basis of the decision to treat using antibiotic prophylaxis.
Undoubtedly, the most relevant finding in our clinical study is the rates
of spontaneous resolution in a large Brazilian cohort.
Because the chance of spontaneous resolution
is as high as 87.5%, 77.6% and 52.8% in VUR grades I, II and III, respectively,
only exceptional cases should undergo primary surgical correction.
The different procedures should be analyzed
for their costs in order to optimize the therapeutic strategy in different
health systems. An individualized strategy seems to be the ultimate goal
and should take into consideration the large number of issues.
CONCLUSION
In conclusion, urinary tract infection is still the major cause of VUR diagnosis. However, early diagnosis and adequate treatment allowed a significantly decrease of morbidity caused by renal injury. The currently employed clinical treatment might be safely used in most of the cases. Spontaneous resolution is directly related to VUR severity and is less likely to occur in grades IV and V for which surgery is a more adequate alternative.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Jodal U, Koskimies O, Hanson E, Lohr G, Olbing H, Smellie J, et al.: Infection pattern in children with vesicoureteral reflux randomly allocated to operation or long-term antibacterial prophylaxis. The International Reflux Study in Children. J Urol. 1992; 148: 1650-2.
- Wingen AM, Koskimies O, Olbing H, Seppanen J, Tamminen-Mobius T: Growth and weight gain in children with vesicoureteral reflux receiving medical versus surgical treatment: 10-year results of a prospective, randomized study. International Reflux Study in Children (European Branch). Acta Paediatr. 1999; 88: 56-61.
- [No authors listed]: Medical versus surgical treatment of primary vesicoureteral reflux: report of the International Reflux Study Committee. Pediatrics. 1981; 67: 392-400.
- Smellie JM: The intravenous urogram in the detection and evaluation of renal damage following urinary tract infection. Pediatr Nephrol. 1995; 9: 213-9; discussion 219-20.
- Goldraich NP, Ramos OL, Goldraich IH: Urography versus DMSA scan in children with vesicoureteric reflux. Pediatr Nephrol. 1989; 3: 1-5.
- Merguerian PA, Jamal MA, Agarwal SK, McLorie GA, Bagli DJ, Shuckett B, et al.: Utility of SPECT DMSA renal scanning in the evaluation of children with primary vesicoureteral reflux. Urology. 1999; 53: 1024-8.
- Bailey RR, Mailing TMJ, Swainson CP: Vesicoureteric reflux and reflux nephropathy. In: Scherier RW, Gottschalk CW (eds.), Disease of the Kidney, Fifth edition. Boston, Litthe, Brown & Co. 1993; pp. 689-727.
- Wheeler D, Vimalachandra D, Hodson EM, Roy LP, Smith G, Craig JC: Antibiotics and surgery for vesicoureteric reflux: a meta-analysis of randomised controlled trials. Arch Dis Child. 2003; 88: 688-94.
- Birminghan Reflux Study Group: Prospective trial of operative versus non operative traitement of severe vesico-ureteric reflux in children: five years observation. Brit Med J. 1987; 295: 237-41.
- Weiss R, Tamminen-Mobius T, Koskimies O, Olbing H, Smellie JM, Hirche H, et al.: Characteristics at entry of children with severe primary vesicoureteral reflux recruited for a multicenter, international therapeutic trial comparing medical and surgical management. The International Reflux Study in Children. J Urol. 1992; 148: 1644-9.
- Scholtmeijer RJ: Treatment of vesicoureteric reflux: results after 3 years in a prospective study. Child Nephrol Urol. 1991; 11: 29-32.
- Greenfield SP, Ng M, Wan J: Experience with vesicoureteral reflux in children: clinical characteristics. J Urol. 1997; 158: 574-7.
- Chand DH, Rhoades T, Poe SA, Kraus S, Strife CF: Incidence and severity of vesicoureteral reflux in children related to age, gender, race and diagnosis. J Urol. 2003; 170: 1548-50.
- Skoog SJ, Belman AB, Majd M: A nonsurgical approach to the management of primary vesicoureteral reflux. J Urol. 1987; 138: 941-6.
- Elder JS, Peters CA, Arant BS Jr, Ewalt DH, Hawtrey CE, Hurwitz RS, et al.: Pediatric Vesicoureteral Reflux Guidelines Panel summary report on the management of primary vesicoureteral reflux in children. J Urol. 1997; 157: 1846-51.
- Arant BS Jr: Medical management of mild and moderate vesicoureteral reflux: followup studies of infants and young children. A preliminary report of the Southwest Pediatric Nephrology Study Group. J Urol. 1992; 148: 1683-7.
- Tamminen-Mobius T, Brunier E, Ebel KD, Lebowitz R, Olbing H, Seppanen U, et al.: Cessation of vesicoureteral reflux for 5 years in infants and children allocated to medical treatment. The International Reflux Study in Children. J Urol. 1992; 148: 1662-6.
- Duckett JW: Vesicoureteral reflux: a ‘conservative’ analysis. Am J Kidney Dis. 1983; 3: 139-44.
- Yeung CK, Godley ML, Dhillon HK, Gordon I, Duffy PG, Ransley PG: The characteristics of primary vesico-ureteric reflux in male and female infants with pre-natal hydronephrosis. Br J Urol. 1997; 80: 319-27.
- Sillen U, Hjalmas K, Aili M, Bjure J, Hanson E, Hansson S: Pronounced detrusor hypercontractility in infants with gross bilateral reflux. J Urol. 1992; 148: 598-9.
____________________
Accepted
after revision:
October 20, 2006
_______________________
Correspondence address:
Dr. Adriano Almeida Calado
Rua Conselheiro Portela, 285 / 602
Recife, PE, 52020-030, Brazil
E-mail: caladourologia@yahoo.com.br