TRAUMATIC
DEGLOVING LESION OF PENILE AND SCROTAL SKIN
(
Download pdf )
LUIZ A. ZANETTINI, ALDO FACHINELLI, GABRIELA P. FONSECA
Section of Urology, University of Caxias do Sul, Rio Grande do Sul, Brazil
ABSTRACT
Avulsions
of penile and scrotal skin are uncommon events and are caused mainly by
accidents with industrial machines and agricultural machine belts.
We report the case of a 30-year old patient
with avulsion and traumatic degloving of the penile and scrotal skin,
with exposure of the cavernous bodies, spongy body, and testes due to
an industrial machine accident. Reconstruction was performed in steps,
achieving a satisfactory esthetic result, normal voiding and reestablished
sexual function.
Key
words: penis; scrotum; wounds and injuries; reconstructive surgical
procedures
Int Braz J Urol. 2005; 31: 262-3
INTRODUCTION
Skin avulsions of male genitals are a rare urological emergency (1). Although not life-threatening, such lesions are incapacitating and psychologically devastating (2) and occur mainly because of accidents with industrial machines or agricultural machine belts (2,3). Avulsions vary from simple lacerations to virtual emasculations (1). Generally, lesions reach only the skin, causing minimal bleeding without producing damage to cavernous bodies, the spongy body or testes (1,2).
CASE REPORT
A
30-year old metallurgist was seen at one municipal hospital in June 2003
suffering from trauma to the external genitalia because of a work accident
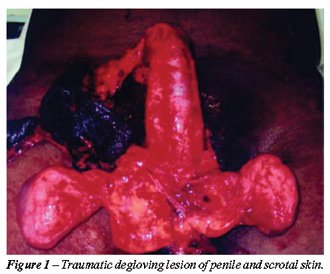
involving industrial machinery. At the emergency room, a total avulsion
of penile and scrotal skin was detected. The skin presenting avulsion
had remained fixed to the penis through a pedicle formed by a flap in
the coronal sulcus, and the skin at the scrotal base had been preserved
(Figure-1).
The patient was taken to the surgery room
approximately 2 hours after the accident. Following peridural anesthesia,
the medical staff performed a careful cleaning, an inventory of lesions
and a debridement of devitalized tissues. The penis was covered again
with the skin attached to the coronal sulcus assuming its viability due
to the pedicle with apparently good vascularization. The left testis was
recovered with remaining skin from the scrotum, and the right testis was
buried in the inguinal region. A small area at the dorsum penis was left
uncovered and the staff preferred to wait for healing by second intention.
Dressings and debridement of devitalized tissues were performed under
anesthesia. After 40 days, the patient underwent re-sectioning of the
cicatricial area at the dorsum penis and a free epidermal graft using
skin from the anterosuperior area of the iliac spine.
Three months after the last procedure, the
patient recovered regular sexual activity. However, he reported painful
erections due to tension and cicatricial retraction of the grafted skin.
Seven months after the accident, the patient
underwent re-sectioning of the free graft scars. The bleeding area of
the penis was covered by rotating the well-vascularized skin from the
penis and scrotum with good esthetic and functional results. On the same
procedure, a right orchiopexy was performed. The remaining scrotal skin
was well vascularized and elastic, and the testis could be properly housed
inside the scrotum (Figure-2).

COMMENTS
Industrial
machine pulleys, chains and rotary discs were responsible for the injury
when they grasped the operator’s clothes and pulled out the skin
of the genital region. The skin was torn at the scrotum, dragging the
skin overlay from the base of the penis while the connection with the
coronal sulcus remaining intact. Part of the scrotal skin was included
in the loose segment. There was no significant blood loss.
After cleaning and debridement of devitalized
tissues, the exposed tissues were covered with viable flaps from the remaining
skin.
When there is no available skin, penile
burial in the scrotum or in the suprapubic region is performed (1). In
the reported case, the posterior portion of the scrotal skin was available
for suture and this tissue was used to cover the left testis and the base
of the penis. At a subsequent stage, we opted for using a free graft to
cover the dorsal bleeding area of the penis. Other techniques, such as
testicular burial in the inguinal region or the inner thigh or expansion
of the scrotal tissue can be employed as well (3).
Among the post-operative complications that
have been reported in the literature are edema, infection, hemorrhage
and cicatricial retraction (2). The treatment of these complications must
be the most conservative possible in order to bring benefits to the patient
(3).
REFERENCES
- Gencosmanoglu R, Bilkay U, Alper M, Gurler T, Cagdas A: Late results of slipt-grafet penoscrotal avulsion injuries. J Trauma. 1995; 39: 1201-3.
- Finical SJ, Arnold PG: Care of the degloved penis and scrotum: a 25-year experience. Plast Reconstr Surg. 1999; 104: 2074-8.
- Paraskevas KI, Anagnostou D, Bouris C: An extensive traumatic degloving lesion of the penis. A case report and review of the literature. Int Urol Nephrol. 2003; 35: 523-7.
_________________________
Received: November 24, 2004
Accepted after revision: March 28, 2005
_______________________
Correspondence
address:
Dr. Luis Alberto Zanettini
Rua Bento Gonçalves, 2048
Caxias do Sul, RS, 95020-410, Brazil
Fax: + 55 54 223-3144
E-mail: urolaz@terra.com.br