MAGNETIC
RESONANCE IMAGING URODYNAMICS. TECHNIQUE DEVELOPMENT AND PRELIMINARY RESULTS
(
Download pdf )
GUSTAVO BORGHESI, ROGERIO SIMONETTI, SUZAN M. GOLDMAN, JACOB SZEJNFELD, MIGUEL SROUGI, VALDEMAR ORTIZ, HOMERO BRUSCHINI
Department of Urology, Federal University of Sao Paulo, UNIFESP, Sao Paulo, SP, Brazil
ABSTRACT
Objectives:
In this preliminary study we report the development of the video urodynamic
technique using magnetic resonance imaging (MRI).
Materials and Methods: We studied 6 women
with genuine stress urinary incontinence, diagnosed by history and physical
examination. Urodynamic examination was performed on multichannel equipment
with the patient in the supine position. Coughing and Valsalva maneuvers
were performed at volumes of 150, 250 and 350 mL. Simultaneously, MRI
was carried out by using 1.5 T GE Signa CV/i high-speed scanner with real
time fluoroscopic imaging possibilities. Fluoroscopic imaging was accomplished
in the corresponding planes with T2-weighted single shot fast spin echo
sequences at a speed of about 1 frame per second. Both studies were recorded
and synchronized, resulting in a single video urodynamic examination.
Results: Dynamic MRI with cine-loop reconstruction
of 1 image per second demonstrated the movement of all compartment of
the relaxed pelvis during straining with the concomitant registration
of abdominal and intravesical pressures. In 5 patients, urinary leakage
was demonstrated during straining and the Valsalva leak point pressure
(VLPP) was determined as the vesical pressure at leak subtracted from
baseline bladder pressure. Mean VLPP was 72.6 cm H2O (ranging from 43
to 122 cm H2O).
Conclusions: The concept of MRI video urodynamics
is feasible. In a clinical perspective, practical aspects represent a
barrier to daily use and it should be recommended for research purposes.
Key
words: urinary incontinence, stress; urodynamics; magnetic resonance
imaging
Int Braz J Urol. 2006; 32: 336-41
INTRODUCTION
Video
urodynamics displaying simultaneous data with radiographic images of the
bladder and urethra were originally described by Miller in 1971 (1). Pressure
flow study combined with fluoroscopy or ultrasonography is generally referred
as video urodynamics, which is currently the gold standard to diagnose
and localize lower urinary tract dysfunction (2).
Magnetic resonance imaging (MRI) with its
noninvasive, nonionizing, multi-planner imaging capabilities offers distinct
advantages over computerized tomography/fluoroscopy and since it has greater
accuracy over ultrasound in the detection of discrete structures, it has
rapidly become a major diagnostic tool in the assessment of pelvic conditions.
Our attention was prompted by the possibility
of using this new modality towards a better understanding of female stress
urinary incontinence (SUI). SUI is the observation of involuntary leakage
of urine from the urethra synchronous with exertion/effort, or sneezing,
or coughing (3). Normally, anatomical support of the bladder neck and
proximal urethra allows the transmission of increased intra-abdominal
pressure to that area of continence, compensating the closure mechanism
and maintaining continence. Leakage occurs as a result of pressure transmission
failure, lack of intact intrinsic mechanism or both (4). However, these
pathophysiological concepts are yet a matter of controversy.
To this date, there has been no satisfactory
investigative method combining observations regarding bladder and urethra
hypermobility, intrinsic sphincter insufficiency, and anatomical pelvic
floor abnormalities in such patients. The fast MRI-systems available have
a capability of functional examinations. Those have been explored and
are currently used for evaluating other organ systems. The possibility
of simultaneous evaluation of bladder and abdominal pressures, bladder
and urethral mobility under effort, and pelvic floor muscles integrity
and disposition, may have a potential role for better understanding SUI
(5). Herein we report this preliminary and innovative effort to develop
this technique.
MATERIALS AND METHODS
After
our Institutional Review Board’s approval and informed consent,
we studied 6 women with genuine stress urinary incontinence, diagnosed
by history and physical examination. Mean age was 53.1 years (range 28
to 70).
Urodynamic examination was performed on
multichannel equipment with the patient in the supine position. Intravesical
pressure was measured by a transurethral 7F double lumen catheter. Abdominal
pressure was measured by a balloon catheter inflated with 5 to 10 mL saline.
Detrusor pressure was indicated by electronically subtracting abdominal
pressure from bladder pressure. Filling cystometry was performed at filling
rate of 50 mL per minute with saline at room temperature. Coughing and
Valsalva maneuvers were performed at volumes of 150, 250 and 350 mL.
Simultaneously, magnetic resonance imaging
was performed by using 1.5 T (Magneton Sonata Maestro Class, Siemens,
Erlangen, Germany) with a 6-channel belt type surface coil placed around
the patient at the level of the symphysis pubis. Morphological T2 true
FISP (true fast imaging with steady-state precession TR 4.5, TE 2.3) weighted
images were taken in sagittal plane during 360 seconds at a speed of 1
frame per second.
Some devices were developed to accomplish
the MRI urodynamics. An especially designed portable polygraph was coupled
to a notebook, together with an adjustable infusion pump. Tube connections
5 meters long were adapted to the system, in order to maintain the electronic
equipments out of the reach of the magnetic field.
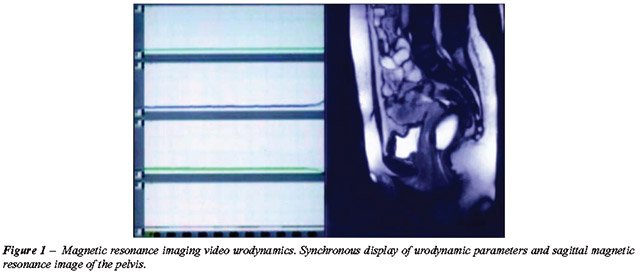
Both studies were recorded and synchronized,
resulting in a single video urodynamic examination (Figure-1).
RESULTS
This
is the report of the last 6 patients when synchronization of both exams
was achieved. Previously, 8 patients were submitted to the MRI video urodynamics
with unsatisfactory results. Although both MRI and urodynamic data were
properly obtained, they were not synchronous making impossible their evaluation
as a single video urodynamic exam.
Mean age was 53.1 years (range 28 to 70).
Table-1 shows patients characteristics.
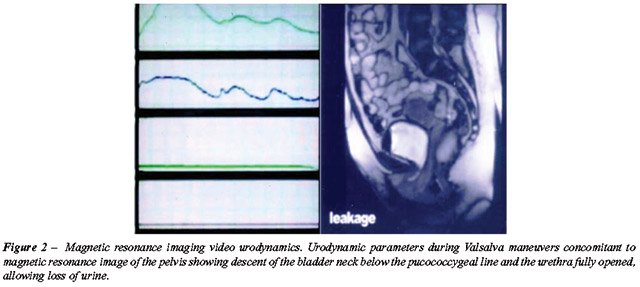
Dynamic MRI with cine-loop reconstruction
of 1 image per second produced images of striking vividness, which demonstrated
the movement of all compartment of the relaxed pelvis during straining
with the concomitant registration of abdominal and intravesical pressures
(Figure-2). In 5 patients, urinary leakage was demonstrated during straining
and the Valsalva leak point pressure (VLPP) was determined as the vesical
pressure at leak subtracted from baseline bladder pressure. Mean VLPP
was 72.6 cm H2O (ranging from 43 to 122 cm H2O) (Figure-2). The recording
of leaking point pressure values simultaneous to the anatomic images of
pelvic floor muscles and bladder base descent under effort was achieved,
providing a new visual dimension to understand SUI.
Urinary leakage was not demonstrated during
MRI urodynamics in only one patient, despite previously demonstrated by
physical examination. No pelvic organ prolapse was observed in this patient,
neither by physical examination nor by MRI. We cannot doubtless state
the reason for this disagreement, but possibly the patient’s inability
to satisfactorily increase intra-abdominal pressure during cough and Valsalva
maneuvers. Patient age (70 years old), and the performance of the exam
in the supine position inside the MRI tunnel with a belt type coil placed
around the patient’s body may have played a role as well.
The pubococcygeal reference line was employed
for diagnosis of descent of the organs. Cystocele was seen in all patients
(4 mild and 2 moderate) and rectocele in only one (moderate). No enterocele
was noted. Pelvic organ prolapse evaluation by MRI correlated well with
the physician examination, except in one patient. Table-2 shows the pelvic
organ prolapse findings by the 2 methods.
Patients accepted well the procedure and
experienced discomfort similar to standard urodynamic test. All patients
said that they would agree to have a similar procedure in the future.
COMMENTS
Recent
studies have changed our understanding of underlying multifactorial causes
to incontinence. Our first understandings supposed that SUI was mainly
a result of descent of the proximal urethra in relation to pelvic floor.
Lately, our attention was focused to the fact that in many women with
bladder dysfunction disorders including incontinence, other facts have
to be considered as specific damage to pelvic muscle ligaments, integrity
of soft connective tissue, peripheral nerves and segmental vessels.
Pelvic floor weakness strongly correlates
with lower urinary tract dysfunction. Stress urinary incontinence often
coexists with pelvic organ prolapse and vice versa. The fact that pelvic
muscle exercises improve urinary control in many women confirms that muscle
action can influence urinary control. The lack of universal success of
such therapy emphasizes the importance of a better understanding of the
relationship among pelvic muscles, pelvic floor fascial structures, bladder
and urethra mobility, and how their damage can lead or contribute to SUI.
Most women with SUI seem to have a combination of urethral dysfunction
and loss of support, and scientific study of these issues awaits insight
into the quantification of each of these parameters as independent variables
(6,7).
In the last 10 years there has been a great
increase in both availability and quality of MRI examinations. Its potential
in the evaluation of pelvic floor disorders is well established. The advantages
of MRI are well known and include the lack of radiation, and the ability
to provide a high-resolution global assessment of the pelvis, its constituent
organs, and the musculofascial support structures. Analysis of the levator
plate complex can be made in the axial and mid-coronal images. Increased
signal intensity of the levator relative to the obturator internus muscle
on proton density images, decreased length, thickness and muscle area
can be used as parameters of levator complex lesion (8,9). Fascial defects
cannot be appreciated on functional cine MRI alone (10). Endoluminal imaging
has the potential to solve the problem regarding urethral support because
a smaller field of view can be used, thereby providing images of higher
spatial resolution. However, it would interfere with the synchronous realization
of the urodynamics.
Functional MRI of the pelvic floor with
depiction of organ movement was first introduced by Yang et al. and Kruyt
et al. in 1991. (11,12). Nevertheless, MRI functional examinations are
still limited in urological practice. The combination of function and
morphology allows for an innovative view of the pelvic floor, and thus
adds to our understanding of the various structure interactions. The intention
of developing a MRI urodynamic examination is the possibility of gathering
the objective functional test of bladder and urethra function provided
by urodynamics with the best anatomical images of the pelvis offered by
MRI. However, this was initially hampered by some practical problems.
The magnetic fields prevent the use of other magnetic material close to
the patient. We had to develop long connections to keep the polygraph
outside the room. The long tunnel in which patients were placed was an
obstacle to routine functional examinations, like having to perform micturition
lying on the table within the MRI. Dynamic MRI has been performed previously
during voiding only in an open MRI system (7). The problems with open
systems are costs and availability, as well as poor spatial and time resolution
compared with closed systems (13). For this reason, in this study, pressure/
flow studies were not performed.
Despite the fact that MRI is considered
to be physically benign, it appears to be associated with psychological
side effects. Patients may experience severe claustrophobia or panic attacks
and others may report milder distress due to the necessity to lie in a
very confined space for a long period. Although all patients in this study
have undergone a MRI procedure for the first time, none of them experienced
significant anxiety. Still, they have not been evaluated with pre and
post-scan specific anxiety questionnaires.
To our knowledge, these preliminary results
represent the first attempt where dynamic MRI has been used during urodynamic
examination.
CONCLUSIONS
The concept of MRI video urodynamics is feasible and the basic technique was achieved after studying the 6 first patients. It is likely to believe that difficulties in some practical aspects represent a barrier to daily use, thus limiting routine clinical studies. However, it brings new possibilities for the study of SUI and bladder dysfunction and represents a useful tool for research purposes and further studies. Clinical research is needed to evaluate the possible diagnostic gains and possible additional use of MRI in urology.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Miller ER: Combined Monitoring for the Study of Continence and Voiding. In: Hinman F (ed.), Hydrodynamics of Micturition. Springfield, Charles C. Thomas. 1971; pp. 5-17.
- Chancellor M, Blaivas J: Synchronous Pressure-Uroflow and Video-Urodynamics. In: Blaivas J, Chancellor M (ed.), Atlas of Urodynamics. Philadelphia, Williams & Wilkins, 1996; pp. 88-104.
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al.: The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003; 61: 37-49.
- Klutke C, Golomb J, Barbaric Z, Raz S: The anatomy of stress incontinence: magnetic resonance imaging of the female bladder neck and urethra. J Urol. 1990; 143: 563-6.
- Mostwin JL, Genadry R, Saunders R, Yang A: Stress incontinence observed with real time sonography and dynamic fastscan magnetic resonance imaging—insights into pathophysiology. Scand J Urol Nephrol Suppl. 2001: 94-9; discussion 106-25.
- DeLancey JO: Stress urinary incontinence: where are we now, where should we go? Am J Obstet Gynecol. 1996; 175: 311-9.
- Hedlund H, Bo K, Lilleas F, Talseth T, Tillung T: The clinical value of dynamic magnetic resonance imaging in normal and incontinent women—a preliminary study on micturition. Scand J Urol Nephrol Suppl. 2001: 87-91; discussion 106-25.
- Tunn R, Paris S, Fischer W, Hamm B, Kuchinke J: Static magnetic resonance imaging of the pelvic floor muscle morphology in women with stress urinary incontinence and pelvic prolapse. Neurourol Urodyn. 1998; 17: 579-89.
- Pannu HK: Magnetic resonance imaging of pelvic organ prolapse. Abdom Imaging. 2002; 27: 660-73.
- Lienemann A, Fischer T: Functional imaging of the pelvic floor. Eur J Radiol. 2003; 47: 117-22.
- Yang A, Mostwin JL, Rosenshein NB, Zerhouni EA: Pelvic floor descent in women: dynamic evaluation with fast MR imaging and cinematic display. Radiology. 1991; 179: 25-33.
- Kruyt RH, Delemarre JB, Doornbos J, Vogel HJ: Normal anorectum: dynamic MR imaging anatomy. Radiology. 1991; 179: 159-63.
- Geitung JT: Magnetic resonance imaging of the pelvic floor—possibilities and present status. Scand J Urol Nephrol Suppl. 2001: 92-3; discussion 106-25.
____________________
Accepted after revision:
April 3, 2006
_______________________
Correspondence address:
Dr. Homero Bruschini
Rua Barata Ribeiro 414 / 35
São Paulo, SP, 01308-000, Brazil
Fax: + 55 11 3218-8282
E-mail: bruschini@uol.com.br
EDITORIAL COMMENT
The authors describe a merging of magnetic resonance imaging and urodynamic technologies. Though fluorourodynamics when initially described was potentially looked upon as an intellectual curiosity, it has since improved into a state-of-the-art method for evaluation of voiding dysfunction. Perhaps with this article we are also observing the emergence of a new marriage of technologies to aid the diagnosis and quantification of bladder dysfunction. Magnetic resonance imaging is already finding a place in the evaluation of pelvic floor prolapse. This extension of application to voiding dysfunction seems to be a reasonably logical step and in retrospect may even be thought of as the obvious natural sequence of diagnostic evolution. It will be unusual if other research groups choose not to examine this process and thus leave these authors known for their sui generis method of patient evaluation. The authors should be credited with their original thoughts and their desire to advance science.
Dr.
Steven P. Petrou
Associate Professor of Urology
Associate Dean, Mayo Clinic College of Medicine
Jacksonville, Florida, USA
E-mail: petrou.steven@mayo.edu