VIDEO
ENDOSCOPIC INGUINAL LYMPHADENECTOMY (VEIL): MINIMALLY INVASIVE RESECTION
OF INGUINAL LYMPH NODES
(
Download pdf )
M. TOBIAS-MACHADO, ALESSANDRO TAVARES, WILSON R. MOLINA JR, PEDRO H. FORSETO JR, ROBERTO V. JULIANO, ERIC R. WROCLAWSKI
Section of Urology, ABC Medical School, Santo Andre, Sao Paulo, Brazil
ABSTRACT
Objectives:
Describe and illustrate a new minimally invasive approach for the radical
resection of inguinal lymph nodes.
Surgical Technique: From the experience
acquired in 7 operated cases, the video endoscopic inguinal lymphadenectomy
(VEIL) technique was standardized in the following surgical steps: 1)
Positioning of the inferior member extended in abduction, 2) Introduction
of 3 work ports distal to the femoral triangle, 3) Expansion of the working
space with gas, 4) Retrograde separation of the skin flap with a harmonic
scalpel, 5) Identification and dissection of the long saphenous vein until
the oval fossa, 6) Identification of the femoral artery, 7) Distal ligature
of the lymph node block at the femoral triangle vertex, 8) Liberation
of the lymph node tissue up to the great vessels above the femoral floor,
9) Distal ligature of the long saphenous vein, 10) Control of the saphenofemoral
junction, 11) Final liberation of the surgical specimen and endoscopic
view showing that all the tissue of the region was resected, 12) Removal
of the surgical specimen through the initial orifice, 13) Vacuum drainage
and synthesis of the incisions.
Comments: The VEIL technique is feasible
and allows the radical removal of inguinal lymph nodes in the same limits
of conventional surgery dissection. The main anatomic repairs of open
surgery can be identified by the endoscopic view, confirming the complete
removal of the lymphatic tissue within the pre-established limits. Preliminary
results suggest that this technique can potentially reduce surgical morbidity.
Oncologic follow-up is yet premature to demonstrate equivalence on the
oncologic point of view.
Key
words: penile cancer; groin; lymphadenectomy; video-assisted
surgery
Int Braz J Urol. 2006; 32: 316-21
INTRODUCTION
Inguinal
lymphadenectomy is indicated in patients presenting penile and urethral
cancer, after local treatment, when there is a lymph node mass that does
not disappear with antibiotic therapy, or when palpable lymph nodes appear
in the postoperative follow-up or when there are risk factors for the
development of inguinal metastasis (prophylactic lymphadenectomy). This
operation is frequently performed through a bilateral inguinal incision
from the iliac crest until the pubic tubercle. There is, however, a high
morbidity regarding the dissected skin flap to access the inguinal lymph
nodes, as well as skin necrosis and local infection, and depending on
the extension of the lymphadenectomy, higher frequency of edema in inferior
members, lymphocele, lymphedema and lymphorea (1).
Trying to reduce the morbidity of this radical
operation the literature shows surgical alternatives that aim at restricting
the inguinal dissection area. However, all techniques present different
local recurrence rates, probably due to false negative results (2).
Video-assisted surgery has been employed
in the iliac and retroperitoneal lymph nodes approach, reducing postoperative
discomfort, minimizing anatomic sequels and allowing a faster recuperation
of patients, keeping the functional results of conventional surgery for
the majority of indications.
We aimed at describing and illustrating
the technical details of a minimally invasive procedure for inguinal lymphadenectomy
recently described in the clinical scenario (3). This technique duplicates
the principles of conventional technique, promoting a radical resection
of inguinal lymph nodes, with encouraging preliminary results regarding
the reduction of surgical morbidity.
SURGICAL TECHNIQUE
The
technique described was developed in a prospective protocol that includes
up to now 7 patients presenting penile spinocellular carcinoma, without
palpable lymph nodes or that had a regression after a 6-week-antibiotic
therapy. All patients had an indication of bilateral lymphadenectomy due
to the presence of risk factors for lymph node dissemination such as:
clinical stage > T1 or information regarding the initial biopsy such
as histological grade > 1, lymphatic or vascular invasion.
After signature of the informed consent
the patients were submitted to classic open surgery in one of the members
(control group) and a video-assisted surgery, named video endoscopic inguinal
lymphadenectomy (VEIL) in the other member (group of the technique to
be assessed).
Control
Member
For the open conventional surgery, we have
used the superficial inguinal lymphadenectomy technique and deep in the
Dressler triangle, medial to the femoral artery, without the preservation
of the long saphenous vein through a large inguinotomy.
Video
Endoscopic Inguinal Lymphadenectomy (VEIL)
1 – Positioning and preparation of
the inferior member - The leg is folded over the thigh in a way to put
in evidence the femoral triangle that is marked with ink over the skin.
After the marking, the leg is extended and fixed to the table with abduction
and light external rotation of the thigh. The video monitor is positioned
at the contralateral side to the operated one at the patient’s pelvic
waist.
2 – Introduction of the ports - At
2 cm of the femoral triangle vertex in a distal sense an incision of 1.5
cm in the skin and in the subcutaneous tissue until the Scarpa’s
fascia is performed, being developed a subcutaneous plan with scissors
and later with a digital maneuver in the largest possible extension. A
second incision of 1 cm, at around 2 cm above and 6 cm medially to the
first incision, to the introduction of a 10 mm port. It is possible to
identify the trajectory of the saphenous vein through this access. A laterally
symmetric position 5 mm port is introduced for graspers, dissection tweezers
and scissors. At the initial access, a 10 mm Hasson trocar is preferably
introduced. All the ports are fixed to the skin through a purse-string
suture with cotton 0. At the initial port, we introduce a 0-degree optic,
and at the medial port, we introduce the tweezers of the harmonic scalpel
and the clipper. The surgeon and the camera operator are positioned laterally
to the operated member.
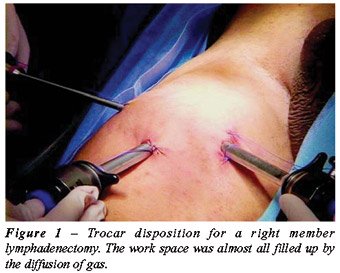
3 – Expansion with gas of the working
space – The creation of a working space is completed through the
initial insufflation of CO2 with a 15-mmHg pressure, with its fast diffusion,
being able to keep the pressure at 5-10 mmHg during the procedure (Figure-1).
Transillumination allows a good orientation regarding the progression
of the dissection area.
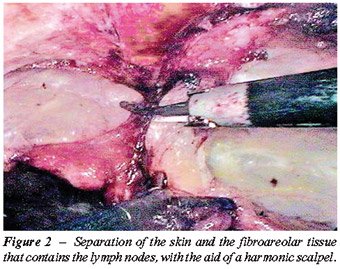
4 – Retrograde separation of the skin
flap – This time is fundamental to the success of the procedure
and is performed with a harmonic scalpel. Initially we perform the separation
between the skin and the fibroareolar tissue that contains the superficial
lymph nodes until the external oblique muscle fascia on the superior part
(Figure-2). Afterwards we proceed to the dissection of the fundamental
parameters, having as a limit the long adductor muscle and its fascia
medially, the sartorius muscle and its fascia laterally, and the inguinal
ligament superiorly. It is possible to identify branches of the femoral
nerve that should be preserved.
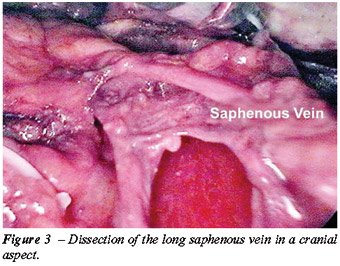
5 – Identification and cranial dissection
of long saphenous vein until the oval fossa (Figure-3).
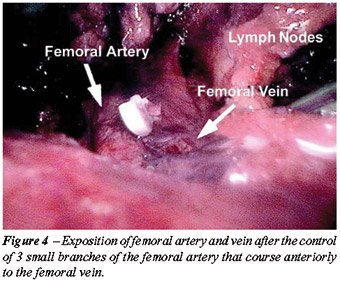
6 – Identification of the femoral
artery – After the identification of the femoral artery and the
opening of the femoral vein sheath we define the lateral limit of the
dissection, allowing the access to the deep cervical lymph nodes (Figure-4).
At this moment it can be necessary to control with 1 or 2 branch clips
coming from the femoral artery that run anteriorly to the femoral vein.
7 – Distal ligature of the lymph node
block at the femoral triangle vertex – the fibroareolar tissue is
dissected with a harmonic scalpel and the control of the final section
at the femoral triangle vertex is obtained with clips.
8 – Liberation of the lymph nodes
until the great vessels above the femoral floor. During this operative
time, the use of the harmonic scalpel and a careful manipulation of the
specimen in areas near the veins are necessary to avoid vascular lesion.
As in the conventional technique, the aim is to skeletonize the femoral
veins, resecting all local lymphatic tissue (Figure-4).
9 – Distal ligature of the long saphenous
vein with clips
10 – Control of the branches and the
long saphenofemoral junction with a harmonic scalpel and metallic clips
- most part of the branches of the long saphenous vein are controlled
only by the harmonic scalpel. Branches larger than 4 mm need clips for
the ligature. The entrance of the long saphenous vein in the femoral vein
should be well dissected and controlled preferably with polymer clips
(Figure-5).

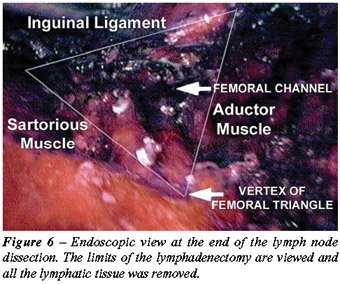
11 – Final liberation of the specimen
medially to the long saphenous vein, ligating the proximal portion of
the lymph nodes at the deep region of the femoral channel with clips.
After completing the liberation of the specimen, the endoscope view attests
that all the tissue of the region was completely resected (Figure-6).
12 – Removal of the surgical specimen
by the 15 mm incision. In case the specimen is of large dimensions, it
can be put inside a bag and latter removed.
13 – Vacuum drainage through the 5
mm orifice and suture of the larger incisions (Figure-7).

COMMENTS
Approximately
30% of the patients with penile spinocellular carcinoma present lymph
node metastasis at the time of the diagnosis. Bilateral inguinal lymphadenectomy
is a procedure accepted as a prognostic and therapeutic value in cases
of penile and urethral spinocellular carcinoma with high risk of developing
metastasis (1). However, morbidity associated to this surgery is high,
being questioned its need mainly when the intention is prophylactic. In
the past, due to the data presented, some centers adopted a conservative
conduct through a rigid clinic follow-up.
Contemporary works have demonstrated that
prophylactic lymphadenectomy offers better survival results than salvage
lymphadenectomy performed in those patients where we have initially opted
for a rigorous observation. Besides that, they have also showed that the
non-controlled lymph node disease was an important cause for morbidity
and mortality in patients with penile cancer.
Before the dilemma of offering radical surgery
with a significant morbidity to 70% of the patients in an unnecessary
way or harm the survival of 30% of the patients submitted to the surveillance
regimen, new alternatives were reported in literature. The techniques
described in the last 20 years to reduce the morbidity are based on the
reduction of inguinal dissection templates. Even though the evident reduction
of operation complications described both with simplified lymphadenectomy
and with the employment of sentinel lymph node with radioisotopes, some
authors believe that its higher morbidity could be related to a rate of
15% of late recurrence of the disease with possible involvement of these
individual’s survival (2).
The present work was motivated by the attempt
to reduce the complications of inguinal lymphadenectomy, based on the
initial works of video-assisted saphenous vein resection, subcutaneous
endoscopic procedures used in plastic surgery and video endoscopic resection
of axillary lymph nodes. (4-6).
Recently, Bishoff et al. described the possibility
of modified dissection of inguinal lymph nodes through endoscopic subcutaneous
access performed in 2 human cadavers and in 1 patient with penile cancer
stage T3N1M0. Dissection was possible on the human cadavers but it was
however not possible in the patient due to the adherence of the enlarged
lymph nodes to the femoral veins (7). After some technical changes we
have performed, to this date, the surgery in a safe and efficient way
in 7 patients with indication of prophylactic lymphadenectomy.
The idealized technique allows a complete
excision of inguinal lymph nodes, the way it is done in conventional surgery,
allowing an initial impression of benefit regarding the lower postoperative
morbidity when compared to the conventional technique. The medium 120
minutes operative time is still superior to the open technique; however,
we should consider the learning curve. Surprisingly enough, there were
no skin complications. The presence of infraumbilical subcutaneous emphysema
of spontaneous resolution is the rule, being uncommon the clinical manifestation.
Hypercarbia can occur intraoperatively, being completely reversible with
hyperventilation, without the need for conversion. In a subjective analysis,
all patients preferred endoscopic surgery. Pathological exam of surgical
specimens showed that the medium number of lymph nodes excised did not
differ from that obtained with conventional surgery.
We attribute this preliminary result to
the following technical principles: 1) Non use of electrical current and
mechanical retraction with subcutaneous retractors. The retraction is
performed atraumatically by the gas, minimizing cutaneous lesions, 2)
Short incisions outside the area of the great vessels allow a shorter
area of lesion of the separated flap and probably less chance of infection,
besides making unnecessary the rotation of the sartorius muscle flap to
recover femoral veins, 3) Control of the lymph nodes, visualized by magnification,
with harmonic scalpel and clips. The proximal and distal ligature of major
channels is fundamental to avoid important lymphoceles or lymphorea.
The presence of skin adherences or palpable
mass of lymph nodes, predictive factors for technical difficulty, were
excluded from this initial study which objectives were to assess the possibility
and technical equivalence to classical lymph nodes resection.
CONCLUSIONS
The
VEIL technique is feasible and allows the radical removal of inguinal
lymph nodes at the same dissection template as conventional surgery. The
main anatomic repairs of open surgery can be identified in an endoscopic
view, confirming the complete removal of the lymphatic tissue within the
pre-established limits.
Preliminary results with this new endoscopic
approach for inguinal lymphadenectomy are promising, with potential to
reduce morbidity. It seems not to change expected oncologic results with
the conventional technique, but the follow-up is still short for definite
conclusions.
Future studies and validation by other authors
will determine the real role of this procedure in the staging and treatment
of patients with penile and urethral spinocellular carcinoma.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Bevan-Thomas R, Slaton JW, Pettaway CA: Contemporary morbidity from lymphadenectomy for penile squamous cell carcinoma: the M.D. Anderson Cancer Center Experience. J Urol. 2002; 167: 1638-42.
- d’Ancona CA, de Lucena RG, Querne FA, Martins MH, Denardi F, Netto NR Jr: Long-term follow-up of penile carcinoma treated with penectomy and bilateral modified inguinal lymphadenectomy. J Urol. 2004; 172: 498-501; discussion 501.
- Machado MT, Tavares A, Molina Jr WR, Zambon JP, Forsetto Jr P, Juliano RV, Wroclawski ER: Comparative study between videoendoscopic radical inguinal lymphadenectomy(VEIL) and standard open lymphadenectomy for penile cancer: preliminary surgical and oncological results. J Urol. 2005; 173: 226, Abst 834.
- Folliguet TA, Le Bret E, Moneta A, Musumeci S, Laborde F: Endoscopic saphenous vein harvesting versus ‘open’ technique. A prospective study. Eur J Cardiothorac Surg. 1998; 13: 662-6.
- Dardour JC, Ktorza T: Endoscopic deep periorbital lifting: study and results based on 50 consecutive cases. Aesthetic Plast Surg. 2000; 24: 292-8.
- Avrahami R, Nudelman I, Watenberg S, Lando O, Hiss Y, Lelchuk S: Minimally invasive surgery for axillary dissection. Cadaveric feasibility study. Surg Endosc. 1998; 12: 466-8.
- Bishoff JA, Lackland AF, Basler JW, Teichman JM, Thompson IM: Endoscopy subcutaneous modified inguinal lymph node dissection (ESMIL) for squamous cell carcinoma of the penis. J Urol. 2003: 169; Supl 4: 78.
____________________
Accepted
after revision:
January 15, 2006
_______________________
Correspondence address:
Dr. Marcos Tobias-Machado
Rua Graúna, 104/131
São Paulo, SP, 04514-000, Brazil
Fax: + 55 11 3288-1003
E-mail: tobias-machado@uol.com.br