STEERABLE
ANTEGRADE STENTING: A NEW TRICK OF THE TRADE
(
Download pdf )
UDO NAGELE, ARISTOTELIS G. ANASTASIADIS, BASTIAN AMEND, DAVID SCHILLING, MARKUS KUCZYK, ARNULF STENZL, KARL-DIETRICH SIEVERT
Department of Urology, University of Tuebingen, Tuebingen, Germany
ABSTRACT
Introduction:
Whereas a retrograde attempt to insert an indwelling stent is performed
in lithotomy position, usually renal access is gained in a prone position.
To overcome the time loss of patient repositioning, a renal puncture can
be performed in a modified lithotomy position with torqued truncus and
slightly elevated flank. There is a two-fold advantage of this position:
transurethral and transrenal access can be obtained using a combined approach.
In the present study, this simple technique is used to position a floppy
guide wire through a modified needle directly through the renal pelvis
into the ureter.
Materials and Methods: The kidney is punctured
in the modified lithotomy position under sonographic control using an
initial three-part puncture needle. A floppy tip guide-wire is inserted
into the collecting system via the needle after retrieving the stylet.
The retracted needle is bent at the tip while the guide-wire is secured
in the needle and the collecting system. The use of the floppy tip guide-wire
helps to insert the curved needle back into the kidney pelvis, which becomes
the precise guidance for the now steerable wire. The desired steerable
stent is positioned under radiographic control in a retrograde fashion
over the endoscopically harbored tip of the guide-wire. Two patient cohorts
(newly described method and conventional method) were compared.
Results: The presented steering procedure
saves 16.5 mean minutes compared to the conventional antegrade stenting
and 79.5 Euros compared to the control group.
Conclusion: The described combined antegrade-retrograde
stent placement through a bent three-part puncture needle results in both
clinical superiority (OR time, success rate) and financial benefits.
Key
words: ureter; stent; nephrostomy; kidney
Int Braz J Urol. 2007; 33: 389-394
INTRODUCTION
Retrograde
ureteral stenting is a daily routine in endourologic procedures. Large
prostatic glands, transitional cell carcinoma of the bladder, impacted
ureteral stones, kidney transplants and orthotopic as well as incontinent
diversions belong to those challenging cases, where a successful retrograde
stenting is not always possible; especially if the ureteral orifice is
involved in a pathological process, antegrade access is sometimes preferable.
The technique of antegrade stent placement
has been in the armamentarium of endourologists for decades. Three critical
steps are necessary to be successful: 1) access of the collecting system,
2) introduction of a guide-wire into the ureter and 3) passage of the
ureteral segment that could not be passed in a retrograde fashion.
Whereas a retrograde attempt to insert an
indwelling stent is normally done in the lithotomy position, usually renal
access is gained in the prone position. To overcome the time loss of patient
repositioning, the renal puncture can be performed in a modified lithotomy
position with a slightly elevated flank. A major advantage of this position
is the combined approach transurethral and transrenal access (1).
This position, in particular, is the easiest
way to gain a safe access below the 12th rib, in the lower
or middle calyx, resulting in an unfavorable angle to the pyeloureteral
junction. Many different techniques are reported to solve this issue,
such as j-shaped ureteral catheters, “cobra” or “hook”-angiographic
catheters, bent wires, peel-away sheets, assistance of rigid or flexible
nephroscopes and dozens of other more or less useful and expensive tools
(2).
This study demonstrates a simple technique
by using only the puncture needle and a floppy guide-wire to pass the
guide-wire into the pyeloureteral junction.
MATERIALS AND METHODS
Patients Recruitment
A
retrospective chart review was performed on 14 consecutive patients receiving
an indwelling ureteral stent using the presented technique, which were
compared to the following 15 consecutive patients, who received the stent
in the conventional technique with the additional nephrostomy tube. Mean
age in this group was 65.5 years (control group 67.5 years). Four patients
had acute urinary retention (control = 6) and 10 had chronic hydronephrosis
(control = 9), caused by malignancy in 6 patients (control = 6) vs. benign
disease in 4 cases (control = 3).
OR time (puncture to successful introduction
of the guide-wire in the ureter), success rate of the intubation of the
proximal ureter, blood transfusions as well as complications in both groups
were recorded and analyzed. Costs for each procedure were recorded and
comparatively evaluated.
Surgical Technique
The
patient is paced in a lithotomy position and the patient is slightly elevated
at the site of the potential kidney puncture (Figure-1). A retrograde
evaluation of the ureter is done. After deciding to use an antegrade or
combined approach to place a ureteral stent, the kidney is punctured under
sonographic control with a three-part puncture needle (Bard GMBH, Karlsruhe,
Germany) 1.3 mm in diameter with MS-cut, thus facilitating visibility
in the ultrasound. Urine is collected for culture before radiopaque contrast
medium is injected into the renal cavity. The renal pelvis, pyeloureteral
junction and calyces are identified; a sensor guide-wire (Boston Scientific,
Nanterre Cedex, France) with a hydrophilic floppy tip is inserted into
the collecting system via the needle after retrieving the stylet.

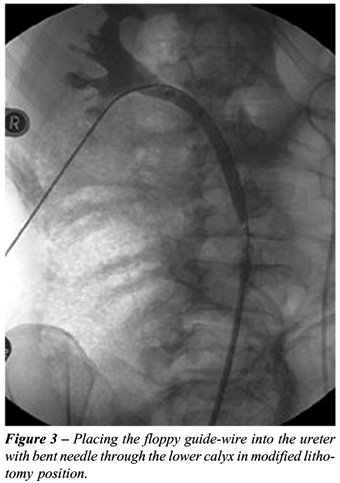
The retracted needle is bent at the tip
at about 3-4 cm length in a smooth curvature (Figure-2) while the guide-wire
is secured in the needle as well as in the collecting system. The use
of the floppy wire results in the possibility of inserting the curved
needle once again into the kidney as the needle acts as a precise guidance
for the now steerable floppy guide-wire (Figure-3).

The wire is guided through the ureter into
the bladder and preferably harbored with an extracting forceps. The end
of the guide-wire is secured with a clamp at the skin level and the desired
steerable stent is positioned under radiographic control in a retrograde
fashion over the harbored tip of the guide-wire. Finally, the wire is
extracted through the puncture and the stent is released in its correct
position.
In the standard technique, a peel-away sheet
is inserted after placing the guide-wire in the calyceal system and either
a “billiard-like” procedure with the floppy wire or an attempt
with angiographic catheters is used to intubate the ureter. After harboring
the guide-wire through the meatus, the stent is placed in the same way
as mentioned above and a 9 Fr. Pigtail nephrostomy is placed in the renal
pelvis for at least one day.
A Foley catheter is placed in the bladder
and a perioperative prophylaxis is administered with a twice-daily oral
application of 250 mg ciprofloxacin.
RESULTS
With
the new procedure, a puncture of the lower calyx was achieved in 7 cases
and the middle calyx or renal pelvis in 7 patients. Direct access into
the ureter was gained in 1 case. In one case, primary access was not possible
due to an infundibulo-ureteral angle of less than 20° (on antegrade
pyelography). After dilatation of the access tract, a metal 15 F nephroscope
sheet was inserted and intubation was facilitated by flexible nephroscopy.
In 10 of the 14 cases, the placement of the wire into the bladder and
therefore combined stenting was possible. After successful stenting, no
nephrostomy tube was required after removal of the guide-wire. OR time
(puncture to intubation of the proximal ureter) was 9.5 minutes.
In the control group, the lower calyx was
punctured in 7 cases and the middle calyx or renal pelvis in 8 cases.
Accidental direct access was gained one time, whereas dilatation of the
nephrostomy tract, insertion of a peel-away sheet and guidance with angiographic
catheters was successful in 9 and aided by flexible ureteroscope (Flex-x,
Storz, Tuttlingen, Germany) in 3 cases. OR time (puncture to intubation
of the proximal ureter) was performed in an average in 26 minutes.
The nephrostomy tube was extracted the first
postoperative day in all cases in the control group.
Mean additive costs in the control cohort
were 79.5 euros. The higher costs were caused by the use of nephrostomy
tube, peel-away sheet, and angiographic catheter.
Mechanical problems of the needles were
not observed after bending (e.g. broken needles, cut wires, etc).
Fever did not occur in either the study
nor in the control group; no major complications were reported and no
blood transfusions were necessary.
COMMENTS
Using
the new torqued lithothomy position facilitates fast access in all patients
including the control group. This technique requires an ultrasound guided
puncture because of the inability to sufficiently contrast the collecting
system in a retrograde fashion. Another positioning with prone split leg
and flank roll position is reported by Grasso et al. (3). The advantages
of the technique described here, compared to the approach of Grasso, are
easier positioning of the patient and facilitated access with semi-rigid
instruments, whereas only radiographic controlled puncture is more difficult.
The use of floppy tip guide-wires avoided
accidental puncture of the contra-lateral wall of the renal pelvis, which
resulted in extravasation and therefore bad vision after application of
radiopaque contrast medium.
Surprisingly, about 7% (n = 1) of initial
guide-wire placements resulted in direct intubation of the ureter in both
patient groups; in all other patients the presented steering procedure
resulted in major time saving (16.5 minutes).
In comparison with another published approach
by a radiologist with a success rate of 88% using pre selected patients,
57% were excluded and a two stage approach was performed later (4). The
presented approach, which has been performed many times, provides the
urologist in even more sophisticated cases (e.g. tumor, stricture etc.)
the potential to perform a one-stage procedure with the possibility of
frequent immediate transurethral intervention.
The use of a combined approach is initially
presented by Wirth et al. (5). The dilatation of the access tract using
the bent needle as a steering guide was less traumatic. This results in
a safe approach to retract the guide-wire without the need of a nephrostomy
or sealing of the tract by gelatine matrix haemostatic sealant (6). The
average cost saving of the steerable approach is 79.5 Euro.
Additional placement of an indwelling stent
in the same session, in case of failed retrograde attempt and without
time loss caused by patient repositioning, further reduces hospital and
especially OR time related costs (2).
CONCLUSION
The described combined antegrade-retrograde stent placement by using a bent initial three-part puncture needle instead of the common equipment and technique of antegrade stenting results a better clinical outcome (OR time, success rate) and financial benefit.
AKNOWLEDGEMENT
Hannes Schramm provided graphical assistence.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Macri A, Magno C, Certo A, Basile A, Scuderi G, Crescenti F, et al.: Combined antegrade and retrograde ureteral stenting: the rendezvous technique. Clin Radiol. 2005; 60: 257-60.
- Watson GM, Patel U: Primary antegrade ureteric stenting: prospective experience and cost-effectiveness analysis in 50 ureters. Clin Radiol. 2001; 56: 568-74.
- Grasso M, Nord R, Bagley DH: Prone split leg and flank roll positioning: simultaneous antegrade and retrograde access to the upper urinary tract. J Endourol. 1993; 7: 307-10.
- Patel U, Abubacker MZ: Ureteral stent placement without postprocedural nephrostomy tube: experience in 41 patients. Radiology. 2004; 230: 435-42.
- Wirth B, Loch T, Papadopoulos I, Schmidt S: Ureteral stenting using a combined antegrade/retrograde procedure. A technique for difficult cases. Scand J Urol Nephrol. 1997; 31: 35-7.
- Nagele U, Schilling D, Kuczyk M, Anastasiadis A, Stenzl A, Sievert K: The use of Floseal® to close the track of the Mini-PCNL shortens the hospital stay. Eur Urol. (suppl) 2005, Abstract 779.
____________________
Accepted
after revision:
March 30, 2007
_______________________
Correspondence
address:
Dr. Udo Nagele
Department of Urology
University of Tuebingen
Hoppe-Seyler-Str. 3
Tuebingen, 72076, Germany
Fax: + 49 7071 295092
E-mail: Udo.Nagele@med.uni-tuebingen.de
EDITORIAL COMMENT
This
paper introduces a technique of antegrade double-J ureteral stent placement
in a single session, for cases in which retrograde access is not possible.
The proposed simultaneous cystoscopic and percutaneous renal access method
affords greater safety compared to antegrade fluoroscopic guidance alone.
The real benefit of positioning the patient
in this manner is that percutaneous access can be obtained if an initial
attempt at retrograde ureteral stenting fails. Traditionally, the patient
would have to be repositioned prone, or awakened for referral to the interventional
radiologists for percutaneous nephrostomy tube placement.
One limitation of this technique is that
some urologists do not routinely perform sonographically guided renal
puncture. Another point of caution is that in the patient with urosepsis
from obstructive uropathy, initial percutaneous nephrostomy drainage is
warranted, rather than trying to place a ureteral stent across the obstructed
segment in a single setting.
Dr.
Sangtae Park
Assistant Professor, Department of Urology,
University of Washington
Seattle, Washington, USA
Email: sangtae_park@yahoo.com
EDITORIAL COMMENT
The
combination of retrograde and antegrade procedures for ureteral stenting,
especially in difficult cases, such as patients with ureteral strictures
and urologic lesions, where conventional stenting has failed, has been
previously described in the literature (1,2). The “rendezvous technique”,
as so elegantly described, is a well-established technique in order to
increase the success rates, even in antegrade stenting procedures (3).
The loss of time in repositioning the patient from prone to lithotomy
position is sometimes an issue, particularly in countries where the concept
of reducing operative time is of great importance. The present study,
which is evaluating the potential of a renal access in a slightly modified
lithotomy position, combining transurethral and transrenal approach at
the same time, is worthy of noticing.
The authors are presenting a punctured technique
in a one-stage procedure that seems feasible and convenient to perform,
reducing the time of the process, with the possible accumulation of a
financial benefit. Nevertheless, the exclusive requirement of ultrasound
guidance and the small number of cases, whereas patient selection criteria
were not unequivocally clarified, necessitate the further evaluation of
this method in the field of ureteral stenting.
Antegrade stent placement is a well-established
procedure, which can manage ureteral strictures and obstruction with great
success (4,5). This newly described technique, that facilitates the transurethral
and transrenal approach at the same time, can only offer another valuable
implement to the arsenal of the endourologists and we believe that in
time will prove its merit in selected cases.
REFERENCES
- Wirth B, Loch T, Papadopoulos I, Schmidt S: Ureteral stenting using a combined antegrade/retrograde procedure. A technique for difficult cases. Scand J Urol Nephrol. 1997; 31: 35-7.
- Clark JA, Isaacson S, Pugash RA: Combined retrograde-antegrade ureteral stenting for ureteral fistulae - a single stage procedure without cystoscopy: case report. Can Assoc Radiol J. 1999; 50: 104-6.
- Macri A, Magno C, Certo A, Basile A, Scuderi G, Crescenti F, et al.: Combined antegrade and retrograde ureteral stenting: the rendezvous technique. Clin Radiol. 2005; 60: 257-60.
- Chitale SV, Scott-Barrett S, Ho ET, Burgess NA: The management of ureteric obstruction secondary to malignant pelvic disease. Clin Radiol. 2002; 57: 1118-21.
- Richter F, Irwin RJ, Watson R, Lang E: Endourologic management of malignant ureteral strictures. J Endourol. 2000; 14: 583-7.
Dr.
Evangelos N. Liatsikos
Dr. Theodore Voudoukis
Department of Urology
University of Patras Medical School
Rio, Patras, Greece
E-mail: liatsikos@yahoo.com