THE
MINIARC® SLING SYSTEM IN THE TREATMENT OF FEMALE STRESS URINARY
INCONTINENCE
( Download
pdf )
ANNETT GAURUDER-BURMESTER, GRALF POPKEN
Department of Urogynecology, German Pelvic Floor Center (AGB), Berlin, and Department of Urology, Helios Klinikum Berlin Buch (GP), Berlin, Germany
ABSTRACT
Aims:
To assess the technical feasibility of a new mini-invasive sling procedure
(MiniArc®) and present short-term results in the treatment of female
urinary incontinence.
Materials and Methods: A total of 97 women with
mixed or stress urinary incontinence (SUI) were treated by placement of the new
single-incision sling. Pelvic organ prolapse was graded using the POP-Q system
(pelvic organ prolapse quantification system). Preoperative workup included urodynamic
evaluation, cough stress test and introital ultrasound. Postoperatively, introital
ultrasound was performed to determine residual urine and check tape position.
Quality of life was measured using King’s Health Questionnaire. A voiding
diary and pad count served to verify the patients’ subjective complaints.
Results: The MiniArc® single-incision sling
procedure was the initial intervention in 37 (38.2%) patients and the second
intervention in 60 (61.7%) patients with recurrent incontinence. The cough stress
test was negative in 79 (83.1%) women 6 weeks after the sling procedure and in
74 (77.8%) at 12 months. De novo urge occurred in 32 (36.8%) women. Quality of
life was significantly improved at 12-month follow-up in 65 (69.1%) patients
(p < 0.001). The number of pads decreased significantly from 2.2 to 0.6 (p < 0.001)
after the procedure. One patient developed an hematoma and bladder perforation
occurred in another.
Conclusions: Our short-term clinical results suggest
that the MiniArc® is a safe and effective minimally invasive sling procedure
for treating female SUI. Randomized comparative controlled trials and long-term
results are still required to define the role of the new sling system in comparison
to established mid-urethral tape techniques for treating incontinence.
Key
words: stress incontinence, urinary; suburethral sling;
minimally invasive procedures; quality of life
Int Braz J Urol. 2009; 35: 334-43
INTRODUCTION
As
the population is aging, the medical community is increasingly challenged
with the problem of urinary incontinence. More women (prevalence of
31% to 63%) are affected than men (1). Urinary incontinence can severely
restrict patients in their daily activities and social life. The costs
in terms of healthcare expenditure are a burden on the National Health
System.
Medical advances in the prevention, diagnosis,
and treatment of urinary incontinence mean an improved quality of life for a
large number of women.
Open colposuspension and conventional tape procedures
are considered the most effective interventions for treating female stress urinary
incontinence (SUI) to date. Good long-term results have been reported for both
interventions (2). The TVT (tension-free vaginal tape) procedure is the most
widely used technique for tape placement worldwide. The operation was first described
by Ulmsten et al. in 1996 and aims at restoring continence by placement of a
monofilament polypropylene mesh under the mid-urethra (3). Various complications
have been reported in association with the TVT procedure including bladder perforation,
voiding dysfunction, retropubic hematoma, and injuries to structures of the true
pelvis. A second generation of tapes has been applied using the transobturator
approach, which was developed by Delorme (4) and De Leval (5). This approach
avoids the retropubic space, thereby reducing the risk of inadvertent bladder
and intestinal injury. Moreover, no adhesions are induced in the retropubic space,
which could be important for the feasibility of future interventions. Transobturator
tapes have since been established as the second tape procedure in addition to
the TVT (6,7).
The new MiniArc® single-incision sling procedure
is comparatively less invasive and is used to reduce complications such as bladder
perforation, injury to structures in the true pelvis, and postoperative pain
in the region of the adductor muscles. The MiniArc® mini-sling is an approved
medical device manufactured by American Medical Systems. Data on the outcome
of the mini-sling procedure is still sparse. Tasinen et al. (8) have reported
very poor results one year after surgery using a mini-invasive collagen sling
to treat neurogenic urinary incontinence. Neuman has reported a failure rate
of 7% in a study of 100 women who underwent TVT-SECUR insertion (9) in 13 hospitals.
Transobturator tapes have since become established and are not inferior to the
TVT (10).
The aim of our study was to assess the technical
feasibility of a new mini-invasive sling procedure (MiniArc®) and present
short-term results in the treatment of female urinary incontinence.
MATERIAL AND METHODS
We
studied 97 women with mixed or stress urinary incontinence based on
reported subjective complaints (voiding diary, pad count) and objective
workup by means of urodynamic evaluation as well as physical and imaging
examination, that included: a) tonometry - premature urge at less than
200 mL bladder filling, b) bladder capacity - reduced to less than
350 mL, c) compliance - reduced at a bladder pressure increase of over
2.6 cm H20 per 100 mL bladder filling (11), d) profile at
rest - low-pressure urethra defined as urethral pressure < 10 cm
H20, e) profile during straining, f) cough stress test,
g) pelvic examination, POP-Q (pelvic organ prolapse quantification
system) (10), and h) introital ultrasound (12,13). The patients were
operated on between January 2007 and July 2008. The women with pure
stress urinary incontinence had undergone prior conservative treatment
with biofeedback, electrostimulation, and duloxetine hydrochloride
between January 2007 and July 2008 (Tables-1 and 2).


Of the 97 patients, 79 (81.4%) had pure SUI, 18
(18.6%) mixed urinary incontinence. All patients with mixed incontinence had
sensory urgency (premature first urge without detrusor contraction). Urodynamically
proven urethral insufficiency and a positive cough stress test were present in
all cases. Tonometry findings were unremarkable in all patients without sensory
urge.
Four (4.2%) women had a cystocele (AaBa > +1)
based on the POP-Q system, but, based on their symptoms, only required sling
insertion.
Since it was our intention not to select patients
as regards constitution, prior surgery, concomitant disease, and urodynamic findings,
a retrospective design appeared to be the most suitable approach.
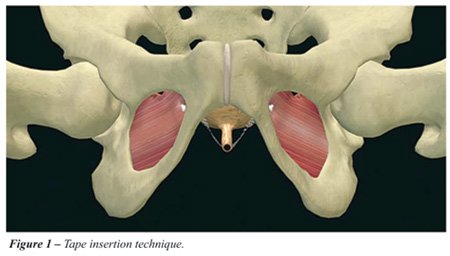
The MiniArc® sling investigated in our study
was 8 cm in length and has self-fixating tips for anchorage in the obturator
internus muscle and membrane (Figures-1 and 2).

All patients were comprehensively informed about
the new procedure by the same person. The transobturator tape was offered as
an alternative approach, and it was emphasized that long-term experience with
the MiniArc? is still lacking. Drawings were presented to the patients to illustrate
the two approaches. Patients were not influenced and could freely select the
method they preferred.
All patients were operated on at the German Pelvic
Floor Center in Berlin. Two experienced operators performed all sling procedures
included in the analysis. Each of them had previously performed the new procedure
in 10 patients not included in the study to become familiar with the technique.
The women included in the study underwent isolated minimally invasive sling insertion
without additional prolapse repair in order to exclude other factors that might
impact the outcome. Patients with mixed urinary incontinence were initially treated
for the urge component using electrostimulation and/or anticholinergic medication
(Table-3).

All surgical interventions were performed in the
lithotomy position under general anesthesia (laryngeal mask). A Foley catheter
was placed and patients received single-shot intraoperative antibiotic prophylaxis
(cephalosporin). The vagina was incised approximately 1.5 - 2 cm below the external
urethral orifice. Next, the paraurethral tissue was dissected with scissors,
creating a tunnel up to the inferior ramus of the pubic bone. The sling was then
advanced into the obturator internus muscle and obturator membrane below the
inferior pubic ramus with a needle. Tension-free positioning of the sling was
ensured by inserting a forceps handle between the tape and the urethra. The insertion
angle was 45 degrees in the direction of the adductor longus muscle tendon (Figure-3).
The vaginal incision was closed with vicryl sutures.

Upon completion of the procedure, the catheter
was removed and the patient had to void spontaneously within the next four hours.
The hospital stay was two days. Postoperative evaluation comprised of the patients’ subjective
assessment (voiding diary, pad count) and quality of life questionnaire. The
clinical evaluation included a pelvic examination, a cough stress test, and introital
ultrasound to measure the postvoid residual urine volume and determine the sling
position.
Follow-up examinations were performed directly
postoperatively as well as 6 weeks and 12 months after tape insertion.
Therapeutic failure was defined as persistent SUI
that impaired the patient’s quality of life and was confirmed by the clinical
findings.
A pad count and a voiding diary served to objectively
ascertain restored continence.
RESULTS
Thirty-seven
(38.2%) patients underwent the MiniArc® procedure as a primary
intervention, 60 (61.7%) for recurrent urinary incontinence. Outcome
differed between these two groups (Table-4).

A low-pressure urethra was diagnosed in 23 patients
(24.2%) and was found to significantly (p < 0.001) correlate with outcome.
Thirteen of the 23 patients (56.5%) in this subgroup were therapeutic failures
with persistent SUI.
The intra- and postoperative complications in the
study population are summarized in (Table-5).

Postoperative voiding dysfunction was defined as
a residual urine volume greater than 100 mL and was treated by alpha-blocker
administration and catheterization.
Patients who developed bladder infection received
cephalosporin for one week.
De novo urge symptoms were treated by anticholinergic
medication in 20 (20.6%) patients and by physical therapy in 12 (12.4%).
The preoperative urge component present in 18 (18.6%)
patients persisted after conservative treatment and the sling procedure in five
(27.8%) cases.
The cough test was negative in 79 (83.1%) women
at 6-week follow-up and in 74 (77.8%) women at 12-month follow-up. The test was
positive in 16 (16.8%) women at 6 weeks and in 20 (21.3%) women at 12 months.
At 12-month follow-up, 77.8% (n = 66) of the women
reported to be continent while 21.3% (n = 20) reported persistent urine loss
during physical activity. These results were also reflected in self-reported
quality of life questionnaires.
Significant improvement in quality of life was
observed for 66 (68.0%) patients at 6-week follow-up (p < 0.001) while 22
(22.7%) had an unchanged quality of life, and 9 (9.4%) reported deterioration
compared with their situation before the intervention. At 12-month follow-up,
there was persistent improvement for 65 (69, 10%) patients (p < 0.001), unchanged
quality of life for 17 (17.5%), and deterioration for 15 (15.5%) women. The number
of pads used decreased significantly from 2.2 before to 0.6 (p < 0.001) after
the sling procedure.
The patients who reported deterioration after the
intervention used more pads than preoperatively, had greater involuntary urine
loss (based on the voiding diary entries), and developed de novo urge (voiding
frequency > 10/day).
Ultrasound was performed to evaluate the postoperative
tape position. The tape was in the area of the mid-urethra in 82 (84.5%) women,
under the distal urethra in 9 (9.3%) women, and close to the bladder neck in
6 patients (6.2%). There was no correlation between tape position and de novo
urge. There was also no correlation between the tape position at ultrasound and
subjectively reported deterioration of incontinence after surgery. The mean length
of surgery was 6 ± 3.5 minutes and the mean blood loss was 10 ± 25
mL.
DISCUSSION
The
results we achieved with the MiniArc® sling system in treating
female urinary incontinence are representative of the short-term outcome
of this new minimally invasive sling procedure. The long-term success
rates (5-10 years) reported in the literature are 78 % (14) to 90%
(14) for colposuspension and 81% for the TVT (15). The outcome reported
for transobturator tapes is comparable to that of the TVT procedure
(16). A new method should be similar or superior to established therapies
and/or be safer and technically easier to handle.
We encountered only one intraoperative hemorrhage,
which did not require blood transfusion, and one bladder perforation, which was
most likely due to scar formation as this patient had already undergone multiple
prior operations. On the whole, the new sling was easy to insert and the duration
of the procedure was very short compared to existing techniques. When the procedure
is properly performed, the risk of injury to the bladder, intestine, or urethra
is negligible. Since the needle is very thin and can be inserted at different
angles, proper advancement requires strict adherence to anatomic structures,
which is why physicians require a training course before performing the procedure
in patients. As with transobturator tapes, the retropubic space is avoided, which
is an advantage if patients need future surgery. Since all interventions were
performed in the setting of a workshop, we opted for standardized anesthesia
with a laryngeal mask. The MiniArc® sling procedure can also be performed
with local anesthesia and analgesia. Further advantages over the transobturator
tape are that there is no risk of obturator nerve damage or adductor muscle pain.
Postprocedural symptoms of overactive bladder are most likely attributable to
the anchorage of the tape. In contrast to TVTs, the self-fixating tip of the
MiniArc® sling does not allow much correction after placement. This is why
the MiniArc® sling should be placed at a distance of 0.5 cm from the mid-urethra
(i.e. the distance between the tape and the urethra) without further intraoperative
tensioning after placement.
The high rate of de novo urge is probably due to
the mode of anchorage of the new tape, which has self-fixating tips. As a result,
tension-free tissue integration is a challenge and depends on numerous factors
such as tissue properties, insertion technique, tape position and retraction.
Despite the standardized technique used in our study, it was not possible to
eliminate de novo urge.
In the patients included in our study, de novo
urge was treated with a combination of anticholinergic medication and physical
therapy. Our findings do not allow any final conclusions to be drawn as to whether
the rather high rate of de novo urge might be lowered by changing the insertion
technique. The cure rates of 83.1.0% after six weeks and 77.8% after 12 months
are good but not comparable to the rates achieved with established tape procedures.
The poorer outcome may be attributable to the large proportion of patients with
recurrent incontinence in our population and the inclusion of 13 (13.6%) patients
with low-pressure urethra. Recurrent incontinence is likely attributable to scar
formation or even rigid tissue integration of the tape, suggesting that the tape
does not provide adequate dynamic support of the urethra. Another possible contributing
factor is neurogenic damage. Established tape procedures are also known to have
poorer results in patients with a low-pressure urethra (17-20), Outcome was poorer
in women with prior incontinence surgery compared with the women who underwent
the MiniArc® procedure as a primary intervention. We did not include a control
group because we wanted each patient to have a choice to opt for any of the conventional
treatments after comprehensive information about the new sling procedure. This
is also why we chose a retrospective design.
The MiniArc® sling can be placed with minimal
tissue injury and is easy to use. However, the instrument design leaves the surgeon
with little control over tape positioning and injury cannot be excluded. Our
preliminary experience suggests that the new tape appears to be associated with
fewer complications in terms of organ damage and bleeding compared with established
tape procedures for treating urinary incontinence.
The indications for MiniArc® insertion will
be defined by its minimal invasiveness and the lower complication rates.
Further studies are needed to determine whether
the new tape is beneficial in women with recurrent urinary incontinence or a
low-pressure urethra. Future studies must also elucidate the causes of the high
rate of de novo urge. Prospective randomized comparative controlled trials and
long-term follow-up are needed to define the relative place of the new sling
system in comparison with other mid-urethral tape techniques used for anti-incontinence
surgery.
The patients who reported deterioration after the
intervention used more pads than preoperatively, had greater involuntary urine
loss (based on the voiding diary entries), and developed de novo urge (voiding
frequency > 10/day).
Thirty-seven (38.2%) patients underwent the MiniArc® procedure
as a primary intervention, 60 (61.7%) for recurrent urinary incontinence. Nevertheless,
there were differences in outcome between these two groups.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Peschers U, Jundt K, Tunn R: Fortschritte in der Diagnostik und Therapie der weiblichen Harninkontinenz. Dtsch Arztebl. 2003; 100: 3322-5.
- Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, et al.: Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical management of female stress urinary incontinence. The American Urological Association. J Urol. 1997; 158: 875-80.
- Ulmsten U, Henriksson L, Johnson P, Varhos G: An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996; 7: 81-5; discussion 85-6.
- Delorme E: Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001; 11: 1306-13.
- de Leval J: Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003; 44: 724-30.
- Barry C, Lim YN, Muller R, Hitchins S, Corstiaans A, Foote A, et al.: A multi-centre, randomised clinical control trial comparing the retropubic (RP) approach versus the transobturator approach (TO) for tension-free, suburethral sling treatment of urodynamic stress incontinence: the TORP study. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19: 171-8.
- Liapis A, Bakas P, Creatsas G: Monarc vs TVT-O for the treatment of primary stress incontinence: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19: 185-90.
- Taskinen S, Fagerholm R, Rintala R: Mini-invasive collagen sling in the treatment of urinary incontinence due to sphincteric incompetence. Int Braz J Urol. 2007; 33: 395-400; discussion 400-6.
- Neuman M: TVT-SECUR: 100 teaching operations with a novel anti-incontinence procedure. Pelviperineology. 2007; 26: 121-3.
- Barber MD, Kleeman S, Karram MM, Paraiso MF, Walters MD, Vasavada S, et al.: Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol. 2008; 111: 611-21.
- International Continence Society: First report on the standardization of terminology of the lower urinary tract function. Br J Urol.1976;48: 39-42.
- Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al.: The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996; 175: 10-7.
- Tunn R, Schaer G, Peschers U, Bader W, Gauruder A, Hanzal E, et al.: Updated recommendations on ultrasonography in urogynecology. Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16: 236-41.
- Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al.: Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004; 23: 190-7.
- Kinn AC: Burch colposuspension for stress urinary incontinence. 5-year results in 153 women. Scand J Urol Nephrol. 1995; 29: 449-55.
- Novara G, Ficarra V, Boscolo-Berto R, Secco S, Cavalleri S, Artibani W: Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol. 2007; 52: 663-78. Erratum in: Eur Urol. 2007; 52: 1548.
- Feyereisl J, Dreher E, Haenggi W, Zikmund J, Schneider H: Long-term results after Burch colposuspension. Am J Obstet Gynecol. 1994; 171: 647-52.
- Ward KL, Hilton P; UK and Ireland TVT Trial Group: Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. BJOG. 2008; 115: 226-33.
- Schär G, Below G, Burkhard F, Peter-Gattlen MC, Schilling J, Schüssler B: Update Expertenbrief.Schlingenoperationen zur Behandlung der weiblichen Stressinkontinenz, 2003. http://www.urogyn.ch/de/download/aug_expert_d.pdf.
- AWMF online. Belastungsinkontinenz der Frau.Leitlinien der Deutschen Gesellschaft für Gynäkologie und Geburtshilfe.Leitlinien-Register Nr.015/005. Entwicklungsstufe 2. http://www.uni-duesseldorf.de/AWMF/ll/015-005.htm.
____________________
Accepted after revision:
February 27, 2009
_______________________
Correspondence address:
Dr. Annett Gauruder-Burmester
German Pelvic Floor Center Berlin
Urogynecology
Friedrichstraße 134
10117 Berlin, Germany
Fax: + 0049 30 4208-7714
E-mail: annett.gauruder@deutschesbeckenbodendzentrum.de
EDITORIAL COMMENT
The evolution of anti-incontinence surgery has
evolved from the retro-pubic colposuspension to the retro-pubic TVT, then to
the trans-obturator TVT and now, possibly, to the mini sub urethral slings. The
background rationale for these changes is the desire to maintain and further
improve the therapeutic results, while reducing the operative related complications.
Given that the current operations for the treatment of female urinary stress
incontinence are far from being perfect in terms of cure and related complications,
and that the industry is moving faster than the clinical trials, one is required
to make personal decisions regarding the exact procedure for their patients with
no sufficient data to rely on. Thus, one should be reluctant to endorse any newly
launched surgical technique, unless appropriate data is provided to support the
efficacy and safety. Moreover, it might be misleading to believe that they the
mini-sling is a very simple procedure to perform – it is not. Extremely
important is proper training with about 20 training operations – and as
for any other new surgical procedure, meticulous theoretical understanding of
the pathophysiology, therapy and complication management and reduction is essential.
Skill maintenance is crucial as well, and this might be achieved by doing 20
operations yearly.
For the time being there are no accepted well structured
indications for different operations for sub-groups of the female urinary incontinent
patients. Some surgeons believe that the retro-pubic TVT are better for the ISD
patients, the trans-obturator for obese patients and the mini-slings for the
old and feeble. This is not supported by reported data, neither are the long
term efficacy and safety of these operations. Multi-centered prospective studies
are essential for providing the world wide urogynecologic community with this
reported data.
Dr.
M. Neuman
Research and Development in Urogynecology
Shaare Zedek Medical Center
Tel-Aviv, Israel
E-mail: mneuman@netvision.net.il
EDITORIAL COMMENT
The
introduction of the intravaginal sling (IVS) in 1996 has revolutionized
the surgical treatment for female stress urinary incontinence (SUI)
(1). Subsequent the minimal invasive suburethral slings replaced the
colposuspension as surgical gold standard for SUI (2). In recent years,
various slings with minor and major modifications have been introduced.
The first major modification was the transobturator slings with reduced
rates of bladder perforation (3,4). Lately the mini-slings followed.
However, do we need this further modification to the existing and what
is possible to improve?
With the mini-slings, external incisions can be
eliminated, only a single vaginal incision is necessary. The mesh became shorter
and no mesh lateral to the obturator is needed. Thus, the tissue trauma can be
reduced and maybe also postoperative pain. The procedure time can possibly be
shorten and less anesthesia are necessary. It is postulated, that the minis-lings
are more minimal invasive than the retropubic and transobturatoric slings.
However, for a new surgical treatment of a non-life-threatening
disease like SIU, the most important issue is to show better results, lower complication
rates and a higher postoperative quality of life and patients´ satisfaction
as the established treatment options.
The first mini-sling, the TVT-secure, showed a
steep learning curve but with some implant challenges and a high variability
in efficacy (5,6).
In the article of Gauruder-Burmester and Popken
results after the implantation of the newest mini-sling, the MiniArc, with a
follow-up until 12 months postoperatively were published. The new sling seems
to be very safe, but the cure rate is not better than the established gold standard.
In addition, the authors report a high rate of de-novo-urgency. However, its
cause remains unclear.
In total, the results look promising, but we need
more data especially long-time data for a final assessment. Thus, prospective
comparative randomized controlled trials with a long follow-up and evaluation
of the quality-of-life and of the postoperative pain are necessary to determine
its true efficacy.
REFERENCES
- Ulmsten U, Petros P: Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol. 1995; 29: 75-82.
- Schröder A, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, Hampel C, Neisius A, Tubaro A, Thüroff JW: Guidelines on Urinary Incontinence. In Aus G (ed), Eau Guidelines. Arnheim, European Association of Urology, 2009, 28-34.
- Delorme E: Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001; 11: 1306-13.
- Novara G, Ficarra V, Boscolo-Berto R, Secco S, Cavalleri S, Artibani W: Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol. 2007; 52: 663-78. Erratum in: Eur Urol. 2007; 52: 1548.
- Meschia M, Barbacini P, Ambrogi V, Pifarotti P, Ricci L, Spreafico L: TVT-secur: a minimally invasive procedure for the treatment of primary stress urinary incontinence. One year data from a multi-centre prospective trial. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20: 313-7.
- Martan A, Svabík K, Masata J, Koleska T, El-Haddad R, Pavlikova M: Initial experience with a short, tension-free vaginal tape (the tension-free vaginal tape secur system). Eur J Obstet Gynecol Reprod Biol. 2009; 143: 121-5.
Dr.
Ricarda M. Bauer
Urologische Klinik und Poliklinik
Ludwig-Maximilians-Universität
München-Grosshadern
München, Germany
E-mail: ricarda.bauer@med.uni-muenchen.de