UROLITHIASIS
IN CHILDREN
(
Download pdf )
PETER-MARTIN BRAUN, CHRISTOPH SEIF, KLAUS-PETER JÜNEMANN, PETER ALKEN(1)
Departments of Urology, University of Kiel, Kiel, and (1)Klinikum Mannheim gGmbH, University of Heidelberg, Mannheim, Germany
ABSTRACT
In general, the criteria for the treatment of urolithiasis in children are the same as those for adults. Today, extracorporeal shock wave lithotripsy (ESWL) is the method of choice in the treatment of most pediatric urinary stones. Stone-free rates between 67% and 93% at short-term follow-up, and 57% to 92% at long-term follow-up, have proven the efficacy of ESWL treatment in children. Nevertheless, the demand for auxiliary measures still remains. In order to achieve the most beneficial success rates under low complications, it is advisable to perform this type of ESWL in centers that claim the experience necessary for ESWL and endourological measures in children.
Key words:
lithiasis; child; lithotripsy; shock-wave therapy
Int Braz J Urol. 2002; 28: 539-44
INTRODUCTION
Since the introduction of ESWL by Chaussy in 1980, the therapeutic strategy for urolithiasis has completely changed. Nowadays, 96% of all urinary stones can be successfully treated by ESWL. In 1986, Newman et al. (1) presented the first reports on ESWL in children. Since then, numerous further reports have been published on the efficiency and safety of ESWL in children (1-31). In contrast to adults, only 1% to 3% of all urinary stones are detected in children. As a result, profound experience in ESWL treatment in children is demanded at all stone centers. Therefore, the number of patients enrolled in each individual study varies between 1 and 73 (7,24,25,30,32-36). One overall survey has been made with 446 children in over 250 stone centers (25). Very few reports have been published that provide exact statistics on the frequency of auxiliary measures in children (7,25,30,32-34,36).
INTERESTING ASPECTS OF ESWL IN CHILDREN
Calyceal
or renal stones with a stone diameter of up to 2cm are an ideal indication
for ESWL. More effective disintegration of even larger stones, together
with swifter and uncomplicated discharge of larger fragments, can be achieved
in children by ESWL. Consequently, ESWL can be indicated for children
with a larger stone volume, and the placement of a ureteral stent before
or after ESWL is generally unnecessary (9,21,29,34).
In our series of 46 children, staghorn stones
were detected in 20%, renal stones with a diameter over 1.5cm in 34%,
and calyceal stones with a diameter of 0.3 to 2.0cm in 29% (7,32). Further
indications for ESWL in combination with endoscopic measures are proximal
and distal ureteral stones that do not pass spontaneously (9,10). However,
potential damage of the gonadal tissue in the ovaries caused by ESWL is
still a controversial subject, and ESWL in female infants is considered
a contraindication by several authors.
LITHOTRIPTER MODIFICATIONS
In
principle, the same ESWL procedure is performed for both children and
adults. Specific modifications depend on the age and size of the child,
and also on the type of lithotripter in use. With the Dornier HM3, a polystyrene
shield was used as lung protection in children smaller than 120cm (14,27-29,34).
Today, no additional equipment is demanded for the treatment of infants
and small children on 2nd and 3rd generation lithotripters (2,7,20,21,23,25,32,36-38)
(Figure-1). The waterbath of the HM3 has been replaced by a multifunctional
table that allows better positioning of children, and uncomplicated treatment
in supine and prone position. The ultrasound location systems and digital
fluoroscopy enable precise location of the stones at lower radiation exposure.
The fluoroscopic screening times in children during treatment for renal
stones averages 2.6 minutes, and for ureteral stones 3.0 minutes (25).
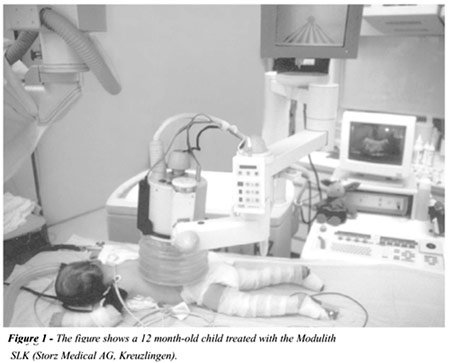
The average radiation exposure for children
is 106.6 (16 to 415) cGy/cm2, and is distinctly lower than 250 cGy/cm2
for adults (11). A further attribute of the new lithotripters enables
the precise focusing of energy on the stone, thus minimizing potential
tissue damage.
ANESTHESIA
Although, nowadays, no general anesthetic is normally administered to adults for ESWL treatment, this is not the case with children. A general anesthetic is demanded in 30% to 100% of children treated by ESWL. However, this demand together with the method of anesthesia varies strongly depending on the age of the child, and on the type of lithotripter in use. The reluctant cooperation of small infants when awake, makes a general anesthetic advisable in this group (2,3,11,13,14,19,24,25,39). The age limit for analgosedation or no anesthetic use at all for children treated by modern lithotripters varies between 3 years (Piezolith) and 12 years (HM3) (21,29,36,40). In our department, children up to the age of 8 years treated by ESWL were routinely given a general anesthetic or preferably, if possible, analgosedation. Only poor compliance necessitated general anesthetics in older children. General anesthesia was administered to 30 out of 46 children (aged 3 months to 14 years). Sixteen children received analgosedation (aged 14 to 17 years). ESWL was performed with the Lithostar Plus (Siemens AG, Erlangen), the Modulith SL20/SLX, and SLK (Storz Medical AG, Kreuzlingen) (Figure-1).
DISINTEGRATION AND STONE-FREE RATES
In
earlier days, the chief aim of stone surgery was to achieve a complete
stone-free condition. Although this does not quite apply to ESWL, long-term
success depends on the stone-free rate. Complete stone disintegration
is achieved in 57% to 97% of cases (1-31), but this is still only a prerequisite
for a stone-free condition. In contrast to adults, more effective disintegration
by ESWL, and subsequent swifter and uncomplicated passage of larger fragments,
has frequently been observed in children (9,21,32,34). The reasons for
this could be that, in general, the dwelling time of stones in children
is only short, the shock wave effect is stronger in children, and they
also quickly recuperate (34) from this method of treatment. Thirty-seven
to 52% of the children were stone free at discharge (7,11,29,32), and
the stone-free rate was between 57% and 97% 3 months after ESWL (1-31),
Table-1.
AUXILIARY MEASURES
The demand for pre- and post-therapeutic auxiliary measures is lower in infants than in older children or adults (11,21-23,27-29,34,38). Large fragments are often easily discharged by infants, thus making stent insertion unnecessary (36). In principle, the auxiliary measures for urinary diversion in complicated hydronephrosis, e.g. ureteral stent and percutaneous nephrostomy (PCN), together with those for stone removal, e.g., ureterorenoscopy (URS) and percutaneous nephrostolithotomy (PCNL), are usually defined as overall auxiliary measures (14,41). However, a distinction must be made, both for adults and children, between these two groups of auxiliary measures. Curative auxiliary measures aim at a stone-free condition. These comprise lithotripsy and stone extraction by URS or PCNL, respectively. Those measures with an adjuvant effect attempt to suppress complications to a minimum, and include the insertion of ureteral stents or percutaneous nephrostomies. Curative auxiliary measures are invasive and must be carried out under general anesthetic, in both younger and older children. Adjuvant measures are less invasive and can frequently be performed under analgosedation. Among our young patients, 19.6% were treated by adjuvant auxiliary procedures, and 8.7% by curative auxiliary measures (7,32). Information on auxiliary measures is rarely given in the bibliography – frequency is reported to be 14 to 37% (25,33-35,39). It must be taken into consideration that retrograde auxiliary measures over URS in boys always bear the risk of damage to the urethra, with subsequent urethral strictures. Hence, whenever possible, this procedure should be avoided in the treatment of boys. Advisable is either repeated ESWL or an antegrade procedures over PCNL. In our patient group, URS was demanded only once for a distal ureteral stone in a small boy (Table-1).
COMPLICATIONS
Petechiea
bleeding at the skin or slight hematuria often arise, whereas severe complications
after ESWL are more seldom in children than in adults. The complication
rate lies between 6% and 26% (2,3,11,25,29,38). Urinary tract infection,
accompanied by a high temperature up to sepsis, is the most common complication
that originates from previously existing, persistent urinary tract infection.
The complication rate in our series of patients was 8%, and these were
all episodes of high temperature from previously existing, persistent
urinary tract infection, caused by upper urinary tract obstruction. These
complications were all conservatively managed by percutaneous procedures
or retrograde ureteral stents plus additional antibiotic therapy (7,32).
Very severe complications that can arise in connection with the infantile
anatomical structure, e.g., pulmonary contusion, hemoptysis or perirenal
hematoma, have only been described in reports on 4 series of patients
(2,13,14,27).
LONG-TERM RESULTS
Stone-free
rate and stone recurrence rate
Only five reports (8,11,18,29,34) have been
made on stone-free rates, between 57% and 92% in a long-term follow-up,
between 18 and 46 months after ESWL in children. A general recurrence
rate of 2% to 44% has been reported for children after ESWL (18,29,34,42),
the residual fragment rate is between 23% and 33% (29,34). In contrast,
the recurrence rate in adults is only between 8% and 10%, and residual
stone growth averages 22% (41). Complex etiology, a high rate of metabolism
disturbances, anatomical changes, and urinary tract infection, are given
as reasons for the higher rate of residual stone growth in children (8,42).
Seventy-two percent of our small patients were stone-free after an average
of 46 months; 5/42 (13.7%) of these developed recurring stones. Residual
stone growth progressed in all 9 children who were not stone-free after
3 months. Either urinary tract infection, metabolic disturbance or an
anatomical change were detected in those children suffering from stone
recurrence or residual stone growth (7,32).
CONCLUSION
Infant
stone patients must be followed over a prolonged period in order to assess
the safety and effectiveness of the treatment strategy. Sonographic and/or
X-ray monitoring of the respective kidney should be performed at least
2 weeks and 3 months after ESWL. Any remaining stubborn residual fragments
are then disintegrated in repeated ESWL treatment.
A metaphylaxis for metabolic disturbances
and a long-term antibiosis for chronic infection are recommended in an
attempt to avoid residual stones. Any existing infrarenal obstruction
must first be cleared.
In order to achieve the most beneficial
success rates under low complications, it is advisable to perform this
type of ESWL in centers that claim the experience necessary for ESWL,
and endourological measures in children.
REFERENCES
- Newman DM, Coury T, Lingeman JE, Mertz JHO, Mosbaugh PG, Steele RE, et al.: Extracorporeal shock wave lithotripsy experience in children. J Urol. 1986; 136: 238–40.
- Abara E, Merguerian PA, McLorie GA, Psihramis KE, Jewett MA, Churchill BM: Lithostar extracorporealshock wave lithotripsy in children. J Urol. 1990; 144: 489–93.
- Adams MC, Newman DM, Lingeman JE: Pediatric ESWL: Long-term results and effects on renal growth. J Endourol. 1989; 3: 245–54.
- Androulakakis PA: Treatment of renal stones in children. Eur Urol Update Series. 1992; 1: 50–4.
- Boddy SA, Kellett MJ, Fletcher MS, Ransley AMI, Paris AM, Whitfield HN, et al.: Extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy in children. J Pediatr Surg. 1987; 22: 223–7.
- Bohle A, Knipper A, Thomas S: Extracorporeal shock wave lithotripsy in pediatric patients. Scand J Urol Nephrol. 1989; 23: 137–40.
- Braun PM, Hoang-Böhm J, Esen T, Krautschick A, Alken P: Therapy of urolithiasis in childhood – ESWL and auxiliary measures. Eur Urol. 1998; 33 (suppl 1): 105.
- Esen T, Bürger R, Witzsch U, Beetz R, Hohenfellner R: Role of metabolic evaluation and specific prophylaxis in the long-term outcome of extracorporeal shock wave lithotripsy in children. J Endourol. 1992; 6: 305–8.
- Frick J, Köhle R, Kunit G: Experience with extracorporeal shock wave lithotripsy in children. Eur Urol. 1988; 14: 181–3.
- Frick J, Sarica K, Kohle R, Kunit G: Long-term follow-up after extracorporeal shockwave lithotripsy in children. Eur Urol. 1991; 19: 225–9.
- Gschwend JE, Paiss T Gottfried HW, Hautmann RE: Extrakorporale Stoßwellenlithotripsie bei Kindern. Komplikationen und Langzeitergebnisse. Urologe A. 1995; 34: 324–8.
- Harmon EP, Neal DE, Thomas R: Pediatric urolithiasis: review of research and current management. Pediatr Nephrol. 1994; 8: 508–12.
- Kramolowsky EV, Willoughby BL, Loening SA: Extracorporeal shock wave lithotripsy in children. J Urol. 1987; 137: 939–41.
- Kroovand RL, Harrison LH, McCullough DL: Extracorporeal shock wave lithotripsy in children. J Urol. 1987; 138: 1106–8.
- Kroovand RL: Stones in pregnancy and in children. J Urol. 1992; 148: 1076–178.
- Lee KW, Rodo-Salas J, Moralales-Fochs L: Course of the urinary lithiasis treatment in the surgery department of a children’s hospital. Cir Pediatr. 1995; 8: 47–50.
- Lim DJ, Walker RD, Ellsworth PI, Newman RC, Co-hen MS, Barraza MA, et al.: Treatment of pediatric urolithiasis between 1984 and 1994. J Urol. 1996; 156: 702–5.
- Lock MT, Speelmann A, Nijman JM, Ackaert KS, Dik P, Scholtmeijer RJ: Experiences with extracorporeal shockwave lithotripsy in 61 children. Ned Tijdschr Geneeskd. 1989; 133: 669–72. Losty P, Surana R, O’Donnell B: Limitations of extracorporeal shock wave lithotripsy for urinary tract calculi in young children. J Pediatr Surg. 1993; 28: 1037–9.
- Lottmann H, Armchanbaud F, Helal B, Mercier-Pageyral B, Melin Y: Extracorporeal shockwavew lithotripsy in children. Study of the effectiveness and renal consequences in a series of eighteen children. Ann Urol Paris. 1995; 29: 136–42.
- Marberger M, Türk C, Steinkogler I: Piezoelectric extracorporeal shock wave lithotripsy in children. J Urol. 1989; 142: 349–52.
- Mininberg D: Extracorporeal shock wave lithotripsy in children: an overview. J Endourol. 1989; 3: 385–9.
- Miroglu C, Tokuc R, Erol H, Tolon J, Erkan A, Bazmanoglu E, et al.: Extracorporeal shock wave lithotripsy in children: report on 79 renal units. J Endourol. 1992; 6: 209–11.
- Mishriki SF, Wills M, Mukherjee A, Frank JD, Feneley RCL: Extracorporeal shock wave lithotripsy for renal calculi in children. Br J Urol. 1992; 69: 303–5.
- Myers DA, Mobley TB, Jenkins JM, Grine WB, Jordan WR: Pediatric low energy lithotripsy with the lithostar. J Urol. 1995; 153: 453–7.
- Sarica K, Kupei S, Sarica N, Gogus O, Kilic S, Saribas S: Long-term follow-up of renal morphology and function in children after lithotripsy. Urol Int. 1995; 54: 95–8.
- Sigman M, Laudone VP, Jenkins AD, Howards SS, Riehle R, Keating MA, et al: Initial experience with extracorporeal shock wave lithotripsy in children. J Urol. 1987; 138: 839–41.
- Schultz-Lampel D, Lazica M, Lampel A, Thüroff JW: ESWL - Treatment of urinary stones in children. J Endourol. 1991; 5: S137.
- Schultz-Lampel D, Lazica M, Lampel A, Bohnen K, Thüroff JW: Langzeitverlauf nach ESWL bei Kindern: Steinfreiheit, Rezidivsteinrate, Blutdruck und Nierenfunktion. Aktuel Urol. 1994; 25: 101–10.
- Zanetti GR, Montanari E, Guarneri A, et al.: Extracorporeal shock wave lithotripsy with MPL 9000 for the treatment of urinary stones in pediatric patients. Arch Ital Urol Androl. 1993; 65: 671–3.
- Zöller G, Waßmann K, Ludewig M, Ringert R-H: Extrakorporale Stoßwellenlithotripsie eines Nierenbeckenausgußsteines bei einem 15 Monate alten Säugling. Aktuel Urol. 1990; 21: 210–3.
- Braun PM, Weber A, Michel MS, Spahn M, Köhrmann KU, Krautschick A, et al.: Are auxiliary measures necessary in therapy of urolithiasis in children? J Endourol. 1998; 12 (suppl 1): 1-8.
- Moreno Aranda J, Cedillo Lopez U, Lopez Pelerano Jl, Hernandez Toriz N, Blanco Bernal SG: Extracorporal lithotripsy in children. Gac Med Mex. 1992; 128: 263-6.
- Nijman JM, Ackaert K, Scholtmeijer RJ, Lock TWTM, Schröder FH: Long-term results of extracorporeal shock wave lithotripsy in children. J Urol. 1989; 142: 609–11.
- Oktay Nazh, Cag Cal, Ceyhun Özyurt, Gürhan Günaydin, Ibrahim Cüreklibatir, Vedat Avcieri, et al.: Results of Extracorporeal shock wave lithotripsy in the pediatric age group. Eur Urol. 1998; 33: 333-6.
- Vandeursen H, Devos P, Baert L : Electromagnetic shock wave lithotripsy in children. J Urol. 1991; 145: 1229–31.
- Lin CM: Extracorporeal shock wave lithotripsy in children: experience with the multifunctional lithotripter MFL 5000. Acta Pediatr Sin. 1992; 33: 357–62.
- Van Horn AC, Hollander JB, Kass EJ: First and second generation lithotripsy in children: results, comparison and follow-up. J Urol. 1995; 153: 1969–71.
- Moazam F, Nazir Z, Jafarey AM: Pediatric urolithiasis: to cut or not to cut. J Pediatr Surg. 1994; 29: 761–4.
- Carvajal-Busslinger MI, Gygi C, Ackermann D, Kaiser G, Bianchetti M: Urolithiasis in childhood. When do what? Eur J Pediatr Surg. 1994 ; 4: 199–200.
- Rassweiler JJ, Köhrmann KU, Seemann O, Tschada R, Alken P: Kidney Stones Medical and Surgical Management. In Coe FC, Favus MJ, Park YC, Parks CH, Preminger GM (eds.), Clinical Comparison of ESWL. Philadelphia, Lippincott Raven Publ. 1996; 571–603.
- Rassweiler JJ, Köhrmann KU, Seemann O, Tschada R, Alken P: Kidney Stones Medical and Surgical Management. In Coe FC, Favus MJ, Park YC, Parks CH, Preminger GM (eds.), Clinical Comparison of ESWL. Philadelphia, Lippincott Raven Publ. 1996; 571–603.
- Diamond DA, Menon M, Lee PH, Rickwood AMK, Johnston JH: Etiological factors in pediatric stone recurrence. J Urol. 1989; 142: 606-8.
___________________
Received: June 6, 2002
Accepted: June 26, 2002
_______________________
Correspondence address:
Dr. Peter-Martin Braun
Urologische Klinik, University Kiel
Arnold-Heller-Str. 7
D-24105 Kiel, Germany
Fax: + 49 431 597-3783
E-mail: pbraun@urology.uni-kiel.de