EXTRACORPOREAL
SHOCKWAVE LITHOTRIPSY VERSUS URETEROSCOPY FOR DISTAL URETERIC CALCULI:
EFFICACY AND PATIENT SATISFACTION
(
Download pdf )
IBRAHIM F. GHALAYINI, MOHAMMED A. AL-GHAZO, YOUSEF S. KHADER
School of Medicine, Jordan University of Science & Technology, King Abdullah University Hospital, Irbid, Jordan
ABSTRACT
Objective:
We compared the efficacy of extracorporeal shock wave lithotripsy (ESWL)
and ureteroscopy (URS) for the treatment of distal ureteral calculi with
respect to patient satisfaction.
Materials and Methods: This is a prospective
study where a total of 212 patients with solitary, radiopaque distal ureteral
calculi were treated with ESWL (n = 92) using Dornier lithotriptor S (MedTech
Europe GmbH) or URS (n = 120). Patient and stone characteristics, treatment
parameters, clinical outcomes, and patient satisfaction were assessed
for each group.
Results: The 2 groups were comparable in
regard to patient age, sex, stone size, and side of treatment. The stone-free
status for ESWL and URS at 3 months was 81.5% and 97.5%, respectively
(p < 0.0001). In addition, 88% of patients who underwent ESWL versus
20% who underwent URS were discharged home the day of procedure. Minor
complications occurred in 3.3% and 8.3% of the ESWL and URS groups, respectively
(p = 0.127). No ureteral perforation or stricture occurred in the URS
group. Postoperative flank pain and dysuria were more severe in the URS
than ESWL group, although the differences were not statistically significant
(p = 0.16). Patient satisfaction was high for both groups, including 94%
for URS and 80% for ESWL (p = 0.002).
Conclusions: URS is more effective than
ESWL for the treatment of distal ureteral calculi. ESWL was more often
performed on an outpatient basis, and showed a trend towards less flank
pain and dysuria, fewer complications and quicker convalescence. Patient
satisfaction was significantly higher for URS according to the questionnaire
used in this study.
Key
words: ureteral calculi; ureteroscopy; extracorporeal shockwave
lithotripsy
Int Braz J Urol. 2006; 32: 656-67
INTRODUCTION
Urinary
lithiasis can cause a greater or lesser degree of obstruction of the lower
ureter, depending on the size of the calculus, urothelial edema and the
degree of impaction, requiring instrumental treatment, sometimes as an
urgent procedure. In the past 25 years, the treatment of these calculi
has evolved from ureterolithotomy to ureterorenoscopy URS (1), extracorporeal
shockwave lithotripsy (ESWL) (2), and endoscopic lithotripsy (3,4).
Advances in the design of the ureteroscope
and ongoing development in ESWL have greatly impacted the management of
ureteric stones (5). The indications for ureteroscopic lithotripsy have
increased with smaller semi-rigid ureteroscopes and reliable laser technology
and the production of more robust flexible instruments has further expanded
the indications for endoscopic intervention. Despite the definite success
of endourological stone treatment, ongoing questions about optimum management
remain debated among urologists.
ESWL and URS are currently accepted treatment
modalities for distal ureteral calculi. Some authors (6,7) favor ESWL
while others (8-10) prefer URS. For both treatment modalities stone-free
rates of more than 90% have been reported (7,9,10).
The American Urological Association Ureteral
Stones Clinical Guidelines Panel has found both to be acceptable treatment
options for patients, based on the stone-free results, morbidity, and
retreatment rates for each respective therapy. However, costs and patient
satisfaction or preference were not addressed (11).
We aim to compare herein the efficacy and
safety of ESWL and URS for distal ureteral calculi with respect to patient
satisfaction.
MATERIALS AND METHODS
A
total of 212 patients undergoing therapy for distal ureteral calculi between
January 2001 and December 2004 were entered into the study. Patients presented
with radiodense ureteral stones distal to the bony pelvis on excretory
urogram or computed tomography (CT) which had not passed spontaneously
within 3 weeks. Patients were included in the study only if the intervention,
either ESWL or URS, was the primary modality and there was a minimum follow-up
period of 3 months. Patients for whom either therapeutic modality was
contraindicated because of pregnancy, urinary tract infection, coagulation
disorders or previous ureteral reimplantation were excluded from the study.
After defining the indications of treatment,
the patients were made aware of both the modalities of treatment and their
probable complications. The need for anesthesia, stent, urethral manipulation,
possible complications, need for repeated follow up especially after ESWL,
and the cost factor involved, were explained to the patient. The patients
were then asked to choose the mode of treatment.
ESWL was performed using the Dornier lithotriptor
S (MedTech Europe GmbH). All patients were positioned prone and the calculi
were localized with fluoroscopic guidance. All patients were given sedatives
and analgesics and the level of shockwave energy was progressively stepped
up till satisfactory stone fragmentation within the patient’s comfort.
URS was performed with rigid 8F Wolf ureteroscope following dilatation
of ureteric orifice if needed. The stones were either extracted via basket
or forceps, or disintegrated with the Pneumatic lithotripsy lithotriptor.
Placement of a ureteral stent at the conclusion of the procedure was left
to the discretion of the treating surgeon. Upon completion of the procedure,
fluoroscopic imaging was performed to determine whether the ureter was
stone-free. All patients were administered prophylactic antibiotic.
Complete stone clearance was assessed at
three months follow up. Patients were followed-up to assess the success
rates and complications of the two procedures. The follow up schedule
was similar in both groups of patients. Plain x-rays were obtained 1,
2, 4 and 6 weeks after discharge and thereafter if residual fragments
persisted. Obstruction of the upper urinary tract was excluded from diagnosis
with the help of ultrasonography. In case of recurrent ureteral colic
or if calculi failed to pass within 6 weeks ureteroscopic stone removal
was performed. Treatment failure was based on the need for further surgical
intervention during follow-up or failure to become stone-free within 3
months (7). At initial follow-up, patients were given a questionnaire,
which we use for all patients with urolithiasis in our center based on
published data about the factors that influenced patient satisfaction
(7,9) (Table-1). Those with total score of 8 or less were considered satisfied
with the procedure. The efficiency quotient (EQ) was calculated using
the formula: Stone free (%) × 100/ (100 + retreatment rate (%) +
rate of auxiliary procedures (%)) (12).
Data were analyzed using Statistical Package
for Social Sciences (SPSS, version 11.5). Pearson’s chi-square,
student t-test, Mann-Whitney U test was used where appropriate and p <
0.05 was considered statistically significant.
RESULTS
One
hundred and twenty patients were treated with URS (male/female: 85/35),
while 92 (male/female: 70/22) patients were treated by ESWL. Patient’s
age varied between 11 and 75 years, with maximum number of patients between
35 to 45 years of age. There were no significant differences in the mean
age, sex ratio and stone size in both groups (Table-2). For the extracorporeal
modality, i.e. ESWL, the mean stone size was 10.4 ± 5.3 mm (range
4 to 27) (Table-2). In this group, 90% received intravenous sedation and
10% general anesthesia. Majority of the patients (88%) had treatments
as an outpatient procedure but all patients needed frequent follow-up
visits. Only 4 patients (4.3%) required pre-ESWL double pigtail stents
for persistent ureteric colic not responding to conservative treatment.
A total of 92 patients required 115 sessions of lithotripsy with average
number of 3720 shock waves at 10-20 kV. Stone-free status at 1 month and
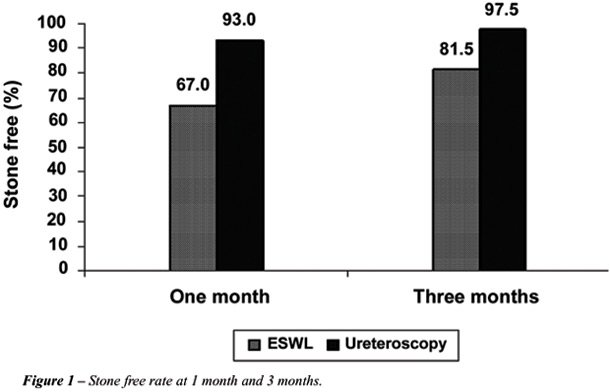
3 month were 67% (n = 62) and 81.5% (n = 75), respectively (Figure-1).
There were no major complications, although three patients (3.3%) developed
fever and infection. In total, 23 patients (25%) required more than one
session of ESWL for disintegration, whereas 17 patients (18.5%) where
ESWL failed were treated by URS for 16 cases and open ureterolithotomy
for one patient with a hard 27 mm stone (Table-3). Of these, there were
4 cases of “steinstrasse” (4%) after ESWL and only 2 were
treated conservatively; the other 2 required URS. EQ at 3 months was 57.
Considerable differences with regard to patient satisfaction were noted
with a mean score of 5.03 ± 3.08. Of the patients 74 (80%) were
satisfied and will recommend the procedure to the others while 18 (20%)
who required re-treatment or URS would opt for URS for recurrence (Table-3).

For the intracorporeal modality, i.e. URS
with pneumatic lithotripsy, the mean stone size was 9.2 ± 5.4 mm
(range, 4 to 27) (Table-2). In this group, 60% of patients had general
anesthesia, 25% local anesthesia and 15% intravenous sedation. The majority
of the patients had treatments as an inpatient procedure (80%) mainly
for ‘social’ reasons, like difficulty in transport. Some of
these were admitted for pain control, infection and stent-related symptoms
but all patients needed less frequent visits for follow-up than ESWL.
After URS, ureteric catheter or double J stent was kept in 41 patients
(34.2%) for 24 hours to 3 weeks. Of these, 12 patients (10%) required
postoperative double-J ureteric stenting due to high stone load. In 28
cases (23%), the calculi could be extracted without fragmentation (forceps
retrieval in 17 and basket retrieval in 11) and all other stones were
fragmented using the Pneumatic lithotripsy lithotriptor. Repeat URS was
however required in 8 patients (6.7%) after 4 weeks (Table-3). EQ at 3
months was 89. In these patients the initial attempt of URS failed due
to failure to adequately dilate the ureteric orifice in six and submucosal
dissection with false passage in two patients. Open surgery was required
for one of these patients who had a hard 25 mm stone. The proximal migration
of calculus occurred in 2 patients (1.7%) who were treated by ESWL. Mean
hospital stay in URS was two days. With respect to complications, there
were 6 cases (5%) of infection in addition to 2 cases of proximal stone
migration and 2 cases of submucosal dissection. No long-term complications,
such as ureteric stricture, were documented during the follow-up period.
Oral pain medication was used in 86% of the URS compared with 74% of ESWL
cases (p = 0.019), for a significantly longer duration (2.4 ± 1.5
versus 1.9 ± 1.5 days, respectively, p = 0.029). Follow-up was
significantly shorter for the URS group (4.2 ± 3.4 versus 5.8 ±
3.0 weeks, p = 0.0001) (Table-3). Stone-free status at 1 month and 3 months
were 93% and 97.5%, respectively (Figure-1). The mean satisfaction score
was 4.03 ± 2.08 which is significantly different from the ESWL
group (p = 0.043). Overall, 113 patients (94%) were completely satisfied
with the therapeutic modality chosen and will recommend it to the others
except for the 7 patients who required re-treatment or open surgery and
preferred to undergo ESWL for recurrence (Table-3).
COMMENTS
Ureteric
stones have a high probability of spontaneous clearance. Spontaneous passage
should be favored if possible (11,13). According to a meta-analysis by
the AUA Guidelines Panel, newly diagnosed stones with a diameter <
5 mm will pass in up to 98%, depending on the degree of obstruction, urothelial
edema and degree of impaction (11). With close controls and in absence
of risk factors like impaired renal function, pain, urinary tract infection
or fever, these stones can be followed safely until spontaneously cleared.
However, most authors recommend not exceeding 4-6 weeks, especially for
obstructive ureteric calculi (14,15). These data show that the success
rate is strongly influenced by the timing of therapeutic intervention
(9). The sooner therapy is initiated, the more stones that might have
passed spontaneously will be treated and, thus, false results in favor
of the chosen procedure will be obtained. In particular small stones have
a high spontaneous passage rate and so therapeutic intervention should
be delayed to allow clearance (9). For this reason treatment was delayed
in our study until 3 weeks after the diagnosis of a prevesical stone unless
earlier therapeutic intervention was mandatory because of recurrent colic.
Peschel et al. (9) have reported on the
differences that they have encountered in dealing with distal ureteral
calculi with both ESWL and URS (rigid or semi-rigid). URS was significantly
better in terms of shorter operative time, fluoroscopy time and time to
achieve a stone free status. The authors recommend URS as first-line treatment
for smaller stones (< 5 mm) that do not pass spontaneously.
In our series patient satisfaction was uniformly
high in both groups but only significantly higher for URS (94 %) compared
to shock wave lithotripsy (80%) (p = 0.002). Also, patient willingness
to undergo a repeated procedure of the same type favored URS. No true
validated instrument exists for comparing patient symptoms and satisfaction
with these different treatment options (16).
The efficacy of the treatment cannot be
only judged by the stone free rate but various other parameters like postoperative
symptoms, patient willingness to undergo a repeated procedure or to recommend
it and the time of return to normal activity. The satisfaction criteria
in this study were more extensive. In our series from the patient viewpoint
achieving a stone-free state as soon as possible is the ultimate goal
once the therapeutic approach has been chosen by most of the patients.
Patient satisfaction generally reflected
treatment success. When assessing the efficacy of treatment an important
consideration is the time it takes to achieve a stone free status. Peschel
et al. (9) also concluded that in this respect there are considerable
differences between ESWL and URS. Results of their patient assessment
clearly demonstrated how important it is to achieve a stone free state
early and even the patients who were free of symptoms said that the awareness
of residual stone fragments and fear of colic were an ever present source
of discomfort and restricted their ability to perform daily activities.
Therefore, most patients in their study were satisfied with URS but would
not be satisfied with ESWL. Pearle et al. (7) found no significant difference
in postoperative symptoms between the 2 treatment groups despite the presence
of a ureteral stent in virtually all patients who underwent URS but only
16% of the ESWL group. Their sample size may preclude statistical significance
but there was a definite trend towards fewer symptoms in regard to bladder
irritability with shock wave lithotripsy. The ESWL group used less pain
medication for a shorter period compared with the URS group, and patient
satisfaction slightly favored ESWL (7). They recommended ESWL with a HM3
lithotripter as first-line treatment for distal stones. In our series,
oral pain medication was used by 74% of the ESWL group compared to 86%
of the URS cases, (p = 0.019), and the duration of analgesic use was significantly
longer in the URS group (p = 0.029). Despite this our patients favored
URS because of the longer time to obtain a stone free status with the
ESWL in addition to the other parameters in the questionnaire. In this
respect our results are in agreement with those of Peschel et al. (9).
From a retrospective review of planned same-day
discharge after ureteroscopy in 114 patients, Wills and Burns (17) concluded
that ureteroscopy should be considered an outpatient procedure. They reported
a 24% immediate admission rate, with about half the admissions for “social”
reasons. The inclusion of social components within our routine assessment
minimizes admission required for social reasons. Our patients have difficulty
in transports as they live far away from the hospital.
Given the high success rates for both treatment
modalities in our study, treatment success must also consider secondary
outcome parameters, such as complications rates, patient satisfaction,
procedural efficacy and cost. Complication rates are low for the treatment
modalities. In neither the series of Pearle et al. (7) or Peschel et al.
(9) did ureteral perforation or stricture occur in either treatment group.
However, ureteral injury is an established, albeit rare, complication
of URS that has never been reported to occur with in situ shock wave lithotripsy.
Furthermore, complications associated with ESWL are generally mild and
related to fragment passage. In our series, although not reaching statistical
significance, an almost 3-fold increase in minor complications occurred
with URS compared to ESWL. Consequently, ESWL is a marginally safer modality
associated with few if any long-term sequelae.
However, the invasiveness of ureteroscopy
cannot be neglected. Before the emergence of modern techniques for stone
fragmentation and newer, better-designed ureteroscopes, complications
like ureteric perforation and avulsion were not uncommon. A comprehensive
review of acute endoscopic injuries reported in the literature from 1984
to 1992 identified 314 ureteric perforations that occurred in 5117 procedures
(6.1%) and complete ureteric avulsion in another 17 procedures, though
infrequent, were documented (0.3%) (18). Harmon et al. (19) observed a
decrease in overall complications from 20% to 12% during a 10-year period
which were attributed to smaller ureteroscopes and increased surgeon’s
experience. Schuster et al. (20) suggested a significant reduction in
ureteric perforation with a less operative time and postoperative complications
with the surgeon’s experience. Proximal migration of stones occurred
in 2 patients (1.7%), which is less than what had been reported. (21,22).
With the emergence of flexible ureteroscopes, migrated stones could be
retrieved with basket. However, these state-of-the-art ureteroscopes are
fragile and experience in our center is still limited. We still use semi-rigid
ureteroscopes for all ureteric calculi.
In our study, only 12 patients (10%) of
the URS group had a double-J ureteric stent inserted for high stone load
while 29 patients (24.2%) had ureteric catheters for 24 hours. This significantly
reduces the occurrence of colic, hematuria and other complications of
obstruction. In the majority of patients undergoing uncomplicated URS
for removal of distal ureteral calculi postoperative discomfort is modest,
lasts less than 2 days and is easily controlled with oral analgesics.
Stricture formation has not been identified. Hence, we do not believe
that routine placement of a ureteral stent following uncomplicated URS
for a distal ureteral calculus is necessary. Routine placement of ureteral
stent after ureteroscopic stone has been considered the standard of care
in most centers but Denstedt et al. (23) performed a prospective trial
of non-stented versus stented ureteroscopic lithotripsy, and concluded
that patients without a stent have significantly fewer symptoms in the
early post-operative period, while there were no differences in terms
of complications and stone free status. In addition it is also important
to notice that with ESWL, more follow-up visits to the clinic were required
until a stone-free state was achieved and at each visit, the patient was
exposed to radiation from plain radiography.
Some investigators concluded that prophylactic
antibiotic during ESWL are unnecessary in patients whose urine before
treatment was sterile (24), other studies showed that antibiotic prophylaxis
with several agents can reduce the rate of bacteriuria significantly (25).
Currently, many urologists routinely prescribe antibiotic prophylaxis
to reduce the potential risk.
On the other hand, an important disadvantage
of URS is that the procedure has to be performed under general or spinal
anesthesia as compared to ESWL, which uses intravenous analgesia. This
exposes the patient to the risks of anesthesia and makes it unfavorable
to patient with significant medical problems but there are some reports
on local anesthesia combined with intravenous sedation for URS (26,27).
From our series local anesthesia with intravenous sedation were sufficiently
effective and safe in our patients with good tolerance. The need for anesthesia
during ESWL depends largely on the energy source. While spark gap lithotripters
(HM-3, MFL 5000) are highly effective, they are also more painful for
the patient, whereas piezoelectric shock wave lithotripsy is associated
to the least pain yet low efficacy. We could not find difficulty in stone
localization under sedation with the Dornier Lithotripter S. We suggest
that the choice of treatment modality for ureteric stones will depend
on the patient since the expertise for both modalities are equally available.
Patient’s factors will include acceptance of invasive procedure,
physical health and preference for earlier stone-free status.
The American Urological Association (AUA)
Guidelines Panel (11) reported its recommendations for the treatment of
ureteric stones. Although this report was clear in its recommendations
of in situ shock wave lithotripsy for the treatment of small ureteral
calculi, it was less clear for the large (> 1 cm) upper ureteric stones.
Although ESWL, URS, percutaneous stone extraction and open surgery were
evaluated as different options; laparoscopic ureterolithotomy was not
mentioned. Indeed, the previously mentioned treatment options have rendered
open procedures a rarity in many hospitals (28). Open surgery was required
for two of our patients with hard large stones. Sharma et al. (29) reported
that open mini-access ureterolithotomy to be a safe and reliable minimally
invasive procedure; its role is mainly confined to salvage for failed
first-line stone treatments but in selected cases, where a poor outcome
can be predicted from other methods, it is an excellent first-line treatment.
Laparoscopy has the advantage of high probability of removing the entire
stone in one procedure, exactly like open surgery.
Success rates for shock wave lithotripsy
may differ according to the lithotriptor used. Average stone-free rate
for cumulative shock wave lithotripsy series in the literature using an
HM3 lithotriptor is slightly but consistently higher than that achieved
with many second and third generation lithotripters and may influence
the choice of treatment (30). It is important to stress that the results
with shock wave lithotripsy are truly machine specific and cannot be translated
to use with other lithotripters (31).
The Dornier Lithotripter S that we use,
proved in different series to be very effective in the treatment of renal
and ureteral calculi (32). Though this is not randomized prospective study,
matching the two groups in terms of age, sex and stone size and studying
consecutive patients managed by the same group of urologists minimize
patient selection bias.
In summary, ESWL offers minimal-invasiveness
but a higher risk of treatment failure compared to URS which reaches immediate
high stone free rates. ESWL is a marginally safer modality associated
with few if any long-term sequelae. Treatment decisions have to be drawn
individually taking into account patients preference, personal experience
and local equipment. We believe that ureteroscopy is preferable to ESWL
for treatment of distal ureteral calculi since it is significantly more
efficient with higher patient satisfaction.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Huffman JL, Bagley DH, Lyon ES: Treatment of distal ureteral calculi using rigid ureteroscope. Urology. 1982; 20: 574-7.
- Chaussy C, Schmiedt E, Jocham D, Brendel W, Forssmann B, Walther V: First clinical experience with extracorporeally induced destruction of kidney stones by shock waves. J Urol. 1982; 127: 417-20.
- Biyani CS, Cornford PA, Powell CS: Ureteroscopic holmium lasertripsy for ureteric stones. Initial experience. Scand J Urol Nephrol. 1998; 32: 92-3.
- Watson GM, Wickham JE: Initial experience with a pulsed dye laser for ureteric calculi. Lancet. 1986; 1: 1357-8.
- Marberger M, Hofbauer J, Turk C, Hobarth K, Albrecht W: Management of ureteric stones. Eur Urol. 1994; 25: 265-72.
- el-Faqih SR, Husain I, Ekman PE, Sharma ND, Chakrabarty A, Talic R: Primary choice of intervention for distal ureteric stone: ureteroscopy or ESWL? Br J Urol. 1988; 62: 13-8.
- Pearle MS, Nadler R, Bercowsky E, Chen C, Dunn M, Figenshau RS, et al.: Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for management of distal ureteral calculi. J Urol. 2001; 166: 1255-60.
- Kapoor DA, Leech JE, Yap WT, Rose JF, Kabler R, Mowad JJ: Cost and efficacy of extracorporeal shock wave lithotripsy versus ureteroscopy in the treatment of lower ureteral calculi. J Urol. 1992; 148: 1095-6.
- Peschel R, Janetschek G, Bartsch G: Extracorporeal shock wave lithotripsy versus ureteroscopy for distal ureteral calculi: a prospective randomized study. J Urol. 1999; 162: 1909-12.
- Segura JW: Ureteroscopy for lower ureteral stones. Urology. 1993; 42: 356-7.
- Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al.: Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. The American Urological Association. J Urol. 1997; 158: 1915-21.
- Ather MH, Memon A: Therapeutic efficacy of Dornier MPL 9000 for prevesical calculi as judged by efficiency quotient. J Endourol. 2000; 14: 551-3.
- Knoll T, Alken P, Michel MS: Progress in Management of Ureteric Stones. EAU Update Series. 2005; 3: 44-50.
- Miller OF, Kane CJ: Time to stone passage for observed ureteral calculi: a guide for patient education. J Urol. 1999; 162: 688-90.
- Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, Gallucci M: Guidelines on urolithiasis. Eur Urol. 2001; 40: 362-71.
- Shah DO, Matlaga BR, Assimos DG: Selecting Treatment for Distal Ureteral Calculi: Shock Wave Lithotripsy versus Ureteroscopy. Rev Urol. 2003; 5: 40-4.
- Wills TE, Burns JR: Ureteroscopy: an outpatient procedure? J Urol. 1994; 151: 1185-7.
- Stoller ML, Wolf J: Endoscopic ureteral injuries. In: McAnich JW (ed.), Traumatic and Reconstructive Urology. Philadelphia, WB Sanders. 1996; pp. 199-205.
- Harmon WJ, Sershon PD, Blute ML, Patterson DE, Segura JW: Ureteroscopy: current practice and long-term complications. J Urol. 1997; 157: 28-32.
- Schuster TG, Hollenbeck BK, Faerber GJ, Wolf JS Jr: Complications of ureteroscopy: analysis of predictive factors. J Urol. 2001; 166: 538-40.
- Fong YK, Ho SH, Peh OH, Ng FC, Lim PH, Quek PL, et al.: Extracorporeal shockwave lithotripsy and intracorporeal lithotripsy for proximal ureteric calculi—a comparative assessment of efficacy and safety. Ann Acad Med Singapore. 2004; 33: 80-3.
- Kelly JD, Keane PF, Johnston SR, Kernohan RM: Laser lithotripsy for ureteric calculi: results in 250 patients. Ulster Med J. 1995; 64: 126-30.
- Denstedt JD, Wollin TA, Sofer M, Nott L, Weir M, D’A Honey RJ: A prospective randomized controlled trial comparing nonstented versus stented ureteroscopic lithotripsy. J Urol. 2001; 165: 1419-22.
- Ilker Y, Turkeri LN, Korten V, Tarcan T, Akdas A: Antimicrobial prophylaxis in management of urinary tract stones by extracorporeal shock-wave lithotripsy: is it necessary? Urology. 1995; 46: 165-7.
- Claes H, Vandeursen R, Baert L: Amoxycillin/clavulanate prophylaxis for extracorporeal shock wave lithotripsy—a comparative study. J Antimicrob Chemother. 1989; 24: 217-20.
- Hosking DH, Smith WE, McColm SE: A comparison of extracorporeal shock wave lithotripsy and ureteroscopy under intravenous sedation for the management of distal ureteric calculi. Can J Urol. 2003; 10: 1780-4.
- Miroglu C, Saporta L: Transurethral ureteroscopy: is local anesthesia with intravenous sedation sufficiently effective and safe? Eur Urol. 1997; 31: 36-9.
- Anagnostou T, Tolley D: Management of ureteric stones. Eur Urol. 2004; 45: 714-21.
- Sharma DM, Maharaj D, Naraynsingh V: Open mini-access ureterolithotomy: the treatment of choice for the refractory ureteric stone? BJU Int. 2003; 92: 614-6.
- Gettman MT, Segura JW: Management of ureteric stones: issues and controversies. BJU Int. 2005; 95: 85-93.
- Hochreiter WW, Danuser H, Perrig M, Studer UE: Extracorporeal shock wave lithotripsy for distal ureteral calculi: what a powerful machine can achieve. J Urol. 2003; 169: 878-80.
- Di Pietro C, Micali S, De Stefani S, Celia A, De Carne C, Bianchi G: Dornier Lithotripter S. The first 50 treatments in our department. Urol Int. 2004; 72: 48-51.
____________________
Accepted after revision:
July 24, 2006
_______________________
Correspondence address:
Dr. Ibrahim Fathi Ghalayini
Associate Professor of Urology
P.O. Box 940165, Amman, 11194, Jordan
Fax: + 00 962 6 568-7422
E-mail: ibrahimg@just.edu.jo
EDITORIAL COMMENT
Ghalayini
and colleagues have prospectively studied the efficacy and patients satisfaction
in a comparative non -randomized study comparing ureteroscopy and shock
wave lithotripsy for distal ureteric stone. An informed consent was taken
and patients opted for one or the other treatment arm.
The
authors have done this study quite amicably and should be congratulated
for the honest description of the results. However, there are several
factors that should be emphasized before incorporating their findings
into every day clinical practice.
Efficacy
of the treatment for distal ureteric stone is judged not only by stone
free rate but other factors like need for re-treatment, ancillary procedure
requirement and admission, all but the last are analyzed by efficient
quotient (1-3). In this work 80% patient falling ureteroscopy required
hospitalization, this is contrary to contemporary experience as admission
following ureteroscopy for distal ureteric stone is only required in a
small minority. Most often it is for social reason, lack of follow-up,
heath care facility (home care, trained general practitioner etc) and
less commonly for complications.
The
other major difference between ureteroscopy and shock wave lithotripsy
is the quantum of complications. The incidence of major complications
like ureteric avulsion and ureteric perforations are fortunately rare
but still a potential possibility. In the present work, the authors have
found a very low incidence of complications in the 2 groups with no major
complication. Need for anesthesia is another major difference between
the 2 procedures. Although in women with distal ureteric calculi requiring
treatment, ureteroscopy could be done under intravenous sedation, in men
the better tolerance of SWL must be weighed against the higher success
rate of ureteroscopy. If both treatment modalities are available, patients
with small distal ureteric calculi, in whom ureteroscopy is likely to
be successful, should be informed of and offered their choice of either
treatment modality. Overall, the study adds nicely to rapidly growing
body of evidence that ureteroscopy is a better option of treatment for
stones moderately large to larger stones (3).
REFERENCES
- Clayman R, McClennan B, Garvin T: Lithostar: An electromagnetic shock wave acoustic unit for extracorporeal lithotripsy. J. Endourol. 1989; 3:307.
- Ather MH, Akhtar S: Appropriate cutoff for treatment of distal ureteral stones by single session in situ extracorporeal shock wave lithotripsy. Urology. 2005; 66: 1165-8.
- Ather MH, Memon A: Therapeutic efficacy of Dornier MPL 9000 for prevesical calculi as judged by efficiency quotient.J Endourol. 2000; 14: 551-3.
Dr. M.
Hammad Ather
Section of Urology, Department of Surgery
Aga Khan University
Karachi, Pakistan
E-mail: hammad.ather@aku.edu
EDITORIAL COMMENT
The
aim of surgical management of ureteral calculi is to obtain complete stone
free state with minimal morbidity to the patient. Ureteral calculi are
often associated with obstruction and treatment should be done to prevent
irreversible damage to the kidney. Mainly 3 factors are important for
the selection of treatment modality. First stone related factors i.e.
stone localization, size, composition, duration, degree of obstruction,
second clinical factors as patient tolerance to intervention, symptomatic
events, patient expectations, infections, solitary kidney, abnormal anatomy
and the third, technical factors i.e. available equipment and cost.
Considerable
progress has been made in the medical and surgical management of urolithiasis
over the past 25 years. Three minimally invasive techniques are currently
available, which significantly reduced the morbidity of stone removal:
percutaneous nephrolithotomy (PNL), rigid and flexible ureterorenoscopy
(URS) and shock wave lithotripsy (SWL). For many clinicians, ureteroscopy
with extraction or intracorporeal lithotripsy is the preferred treatment
of distal ureteral calculi. However, shock wave lithotripsy with or without
stent implantation is the treatment of choice in some centers. Studies
suggest that either SWL or URS are useful options for the management of
distal ureteral calculi. Ureteroscopic access is frequently useful for
the management of ureteral calculi when shock wave lithotripsy is failed
and for complex calculi because shock wave lithotripsy is not the ideal
modality for the management of this kind of calculi. Several investigators
do not advocate the use of shock wave lithotripsy for the treatment of
distal and prevesicular stones due to difficult positioning of the patients
for these procedures in which prone or modified sitting position is preferred
in these situations. The advances in the fiber optic lens systems resulted
in the manufacturing of smaller ureteroscopic instruments, which enabled
widespread use of routine diagnostic and therapeutic procedures within
the ureter and kidney. Open surgery is rarely preferred today but it remains
as an option for a salvage procedure. Alternatively laparoscopic surgery
is a minimally invasive option that can be used in circumstances where
open surgery may have been indicated.
As
this study showed URS and ESWL modalities share an overall high success
rate with low morbidity and both modalities has also proven to be effective
and safe therefore the selection of the optimal treatment for distal ureteral
calculi remains one of the most controversial issues currently in endourology.
Although
ureterecospic treatment is more invasive than ESWL the patient may achieve
a stone free status with a single procedure. ESWL is less invasive but
a drawback from the patients’ perspective may be the long follow-up
until a stone free state or the risk of a requirement for additional invasive
procedures and retreatment need associated with ESWL. Conversely patient
may favor ESWL because of fear of the anesthesia requirement associated
with ureteroscopy and the possibility of a temporary ureteral stent implementation.
ESWL can be done as an outpatient procedure with sedation.
ESWL
is equivalent to URS for smaller stones (less than 1 cm) but becomes significantly
less efficient with larger stones. Generally ESWL was recommended for
small and solitary stones, and URS for large or multiple stones. Not expectedly,
smaller stones (less than 5 mm) that had not passed spontaneously by 3
weeks can be more efficiently treated with URS, because they are the most
difficult to localize and focus with ESWL.
A
review of the literature revealed that the mean stone free rate for ESWL
are 50-95% and for ureteroscopy 96-100%, retreatment rates are 27-50%
for ESWL and 0.8-19% for ureteroscopy.
Recent
studies suggest a tendency from noninvasive ESWL to ureteroscopy. As depicted
in the current study patient satisfaction is also better in URS.
Choice
of treatment modality depends on the current data regarding effectivity,
complications and cost-effectiveness, physicians’ expertise and
available equipment. The patients preferences as anesthesia acceptance
or deny and immediate cure expectations are also the factors that effecting
the choice. The patient should be informed for the existing active treatment
modalities and their relative benefits and risks.
REFERENCES
- Ceylan K, Sunbul O, Sahin A, Gunes M: Ureteroscopic treatment of ureteral lithiasis with pneumatic lithotripsy: analysis of 287 procedures in a public hospital. Urol Res. 2005; 33: 422-5.
- Kupeli B, Biri H, Isen K, Onaran M, Alkibay T, Karaoglan U, Bozkirli I: Treatment of ureteral stones: comparison of extracorporeal shock wave lithotripsy and endourologic alternatives. Eur Urol. 1998; 34: 474-9.
- Peschel R, Janetschek G, Bartsch G: Extracorporeal shock wave lithotripsy versus ureteroscopy for distal ureteral calculi: a prospective randomized study. J Urol. 1999; 162: 1909-12.
- Shah DO, Matlaga BR, Assimos DG: Selecting treatment for distal ureteral calculi: shock wave lithotripsy versus ureteroscopy. Rev Urol. 2003; 5: 40-4.
Dr. Kadir
Ceylan
Department of Urology, School of Medicine
Yuzuncu Yil University
Van, Turkey
E-mail: drceylan26@yahoo.com
EDITORIAL COMMENT
The optimal treatment for distal ureteral stones remains an important question in urology. While there have been multiple studies addressing this issue, there have been only 2 prospective randomized trials to date, each with a contradictory answer. In a multi-institutional trial Pearle et al. (1) concluded that shock wave lithotripsy is preferable while Peschel et al. (2) instead determined that ureteroscopy should be first line treatment. Of note, these conclusions were not based on stone free rates alone, but instead included results from patient questionnaires addressing postoperative pain and satisfaction. Due to its non-randomized study design and inherent risk of selection bias, this work by Ghalayini and colleagues does not provide the definitive answer for the treatment of distal ureteral stones. However, it does provide an interesting insight into what patients find important regarding their procedure. Despite taking significantly less oral pain medication for a shorter period of time and having fewer complications, patients in the shock wave lithotripsy group had a lower level of satisfaction than patients undergoing ureteroscopy. It is important to note that the questionnaire used to obtain these results has not been validated, but it is clear that the global assessment of patient satisfaction was composed of more than just postoperative discomfort. The authors suggest that the decreased satisfaction in the shock wave lithotripsy group was due to the more prolonged time for stone passage relative to ureteroscopy. While no analysis was performed directly addressing this conclusion, shorter time to stone passage following ureteroscopy is a possible explanation as to why patients favored a procedure that was clearly more painful. Definitive proof supporting this conclusion will require further study, but when counseling patients on shock wave lithotripsy versus ureteroscopy for treatment of distal ureteral stones, the patient’s feelings regarding stone passage time may help suggest one procedure over the other.
REFERENCES
- Pearle MS, Nadler R, Bercowsky E, Chen C, Dunn M, Figenshau RS, et al.: Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for management of distal ureteral calculi. J Urol. 2001; 166: 1255-60.
- Peschel R, Janetschek G, Bartsch G: Extracorporeal shock wave lithotripsy versus ureteroscopy for distal ureteral calculi: a prospective randomized study. J Urol. 1999; 162: 1909-12.
Dr. Kyle Anderson
Dept of Urology, Section of Endourology
University of Minnesota
Edina, Minnesota, USA