SPLENOSIS.
A DIAGNOSIS TO BE CONSIDERED
(
Download pdf )
JORGE C. RIBEIRO, CARLOS M. SILVA, AMERICO R. SANTOS
Section of Urology, São Marcos Hospital, Braga, Portugal
ABSTRACT
The term splenosis applies to the autotransplanted splenic tissue resulting from seeding in the context of past splenic trauma or surgery. We report a 42-year-old man with a history of splenectomy observed for an incidentally found retrovesical mass thought to be an ectopic testicle. The abdominal laparotomy revealed multiple focuses of pelvic splenosis. As splenosis can be diagnosed through specific imaging studies one should always consider it in differential diagnosis of a mass discovered years after splenic surgery or trauma.
Key
words: spleen; wounds and injuries; splenosis; bladder
Int Braz J Urol. 2006; 32: 678-80
INTRODUCTION
Ectopic
splenic tissue is a cause of incidentally found mass leading to diagnostic
confusion. It can present as a congenital accessory spleen typically localized
medially to the orthotropic spleen or as a mass detected several years
after a splenic surgery or trauma. These implants, resulting from seeding,
can mimic a neoplasm. However, specific diagnostic tests can confirm diagnosis
and avoid unnecessary surgery.
In this paper we discuss a case of an incidental
retrovesical mass in a patient with an absent left testicle that lead
us to think of an ectopic testicle.
CASE REPORT
A
42 year-old male patient with a history of Behçet disease and a
motor vehicle accident 20 years before resulting in emergent splenectomy,
was referred due to an incidental retrovesical mass. A routine abdominal
ultrasound detected a solid retrovesical neoformation independent from
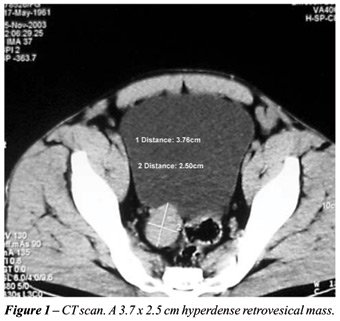
seminal vesicles. The CT scan confirmed a 3.7 x 2.5 cm mass (Figure-1).
No mass was identifiable on abdominal palpation
or rectal exam. The left testicle was absent. IVU, transrectal ultrasound,
and urethrocistoscopy were normal. The hypothesis of an ectopic left testicle
tumor emerged. Testis tumor markers (DHL, ß-HCG and α-FP) were
within normal range.
A pelvic MRI was ordered and revealed a
nodular structure with 3.7 x 2.8 cm, morphologically ovoid, paramedially
and superiorly to seminal vesicles, medially to the sigmoid colon and
independently from these structures. Its lobulated contour with intermediate
signal on T1, similar to muscle, and hyper signal on T2, superior to muscle
and inferior to fat, were against a testicle but uncertainty on the nature
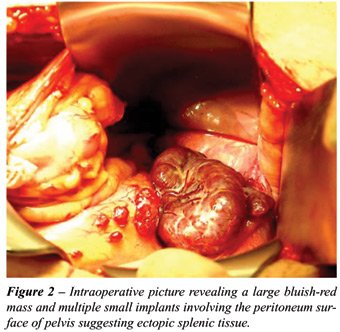
of the lesion remained. An open abdominal laparotomy was performed. Multiple
bluish-red nodules scattered through the pelvis involving both visceral
and parietal peritoneal surfaces, suggested ectopic splenic tissue (Figure-2).
The histological exam confirmed splenosis.
COMMENTS
Splenosis
affects one to two thirds of patients submitted to splenectomy for trauma
(1). Implantation from seeding is most frequently in serosal surfaces
of small and large intestine, greater omentum, parietal peritoneum, mesentery,
diaphragm undersurface and more rarely, in cases of severe trauma, intrahepatic
or even intrathoracic (2,3).
Although splenosis can seldom present as
a vague abdominal or testicular pain, intestinal obstruction from adhesions,
GI bleeding and spontaneous rupture, it usually is an incidental finding
during surgery, either laparoscopy or imaging (2).
When present as an incidental imaging mass
it has been reported on to mimic renal, adrenal or abdominal tumors, metastases,
lymphoma, endometriosis and ectopic testicles (1-4). Although usual imaging
modalities (US, CT, MRI) are helpful to localize and determine the size,
structure and relations with adjacent organs they are not specific.
If we had considered splenosis, signs of
residual splenic tissue as the absence of Howell-Jolly bodies, siderocytes,
Heinz bodies and pitted red cells on peripheral blood smear a could have
been of help, but their presence is still possible due to less functioning
splenosis tissue (2,3)
More specific and diagnostic studies using
agents that are sequestered by reticulendothelial tissue, like 99mtechnetium
sufur colloid, 99mtechnetium labeled heat-denatured autologous
red blood cells or 111In-labeled platelets scans (1,2) and recently ferumoxide-enhanced
MRI (4) have been used.
In conclusion, all patients with a history
of spleen surgery or trauma should consider the hypothesis of splenosis
in differential diagnosis of a newly found mass.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Pumberger W, Wiesbauer P, Leitha T: Splenosis mimicking tumor recurrence in renal cell carcinoma: detection on selective spleen scintigraphy. J Pediatr Surg. 2001; 36: 1089-91.
- Khosravi MR, Margulies DR, Alsabeh R, Nissen N, Phillips EH, Morgenstern L: Consider the diagnosis of splenosis for soft tissue masses long after any splenic injury. Am Surg. 2004; 70: 967-70.
- Weinstein RP, Genega EM, Dalbagni G: Splenosis mimicking transitional cell carcinoma. J Urol. 1999; 161: 1281.
- Berman AJ, Zahalsky MP, Okon SA, Wagner JR: Distinguishing splenosis from renal masses using ferumoxide-enhanced magnetic resonance imaging. Urology. 2003; 62: 748.
____________________
Accepted after revision:
March 25, 2006
_______________________
Correspondence
address:
Dr. Jorge Cabral Ribeiro
Hospital de São Marcos, Section of Urology
Apartado 2242
Braga, 4701-965, Portugal
Fax: + 35 125-3613334
E-mail: jcabralribeiro@netcabo.pt