CHILDHOOD
RENAL LYMPHANGIECTASIA
(
Download pdf )
To the Editor:
An
asymptomatic 4 month-old white female had a 2 x 3 cm faint birthmark on
her mid-thoracic back consistent with a cutaneous telangiectasia. MRI
of the spine incidentally demonstrated an infiltrative right renal lesion.
Ultrasound showed an infiltrative lesion in the enlarged right kidney
and proximal ipsilateral ureter as well as heterogeneously increased renal
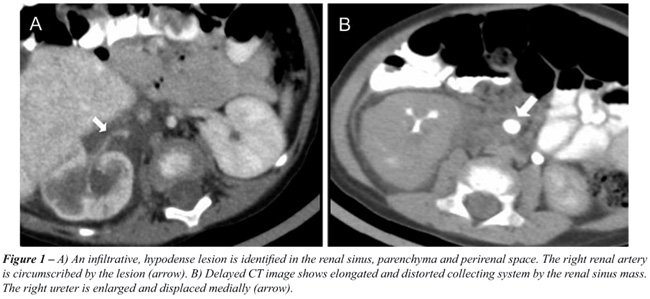
cortical echogenicity. Abdominal CT scan revealed a hypodense lesion (Hounsfield
units from 0 to +20) infiltrating the renal pelvis and parenchyma, circumscribing
the right kidney and proximal ureter (Figure-1, A). Delayed contrast images
showed compression of the ureterovesical junction with medial displacement
of the right ureter (Figure-1, B). Abdominal MRI characterized the lesion
as heterogenously hyperintense and hypointense on T2 and T1 weighted images,
respectively (Figure-2). Right kidney differential function was 28% by
MAG-3 renal scan. The infiltrative character of the lesion without significant
enhancement is consistent with a renal lymphangiectasia. At 2.5 years
of follow-up, she remains asymptomatic without radiological change.

Renal lymphangiectasia is a rare, benign
condition characterized by developmental malformation of the perirenal
lymphatic system. The lymphatic structures that surround the kidney fail
to establish normal communication with the rest of the lymphatic system.
The physiopathological process is ectasia of lymphatic vessels without
obstruction (1,2). It can be focal, unilateral or bilateral and may be
found in pediatric or adult patients. There are reports of familial predisposition
(2). Like other lymphatic lesions, renal lymphangiectasia can appear suddenly,
grow rapidly, cease growth abruptly, or even regress spontaneously. Signs
and symptoms may vary from none to microscopic or macroscopic hematuria,
proteinuria, flank pain, abdominal pain/distension, palpable abdominal
mass, lower extremity edema and hypertension. Renal function is generally
preserved.
Radiological imaging modalities have aided
diagnosis, including renal US, IVP, CT, and MRI. Renal US can show an
enlarged and lobulated kidney with increased echogenicity and loss of
normal corticomedullary differentiation (2). The CT scan reveals multilocular
cyst/fluid filled masses with thin walls in the perirenal and parapelvic
region. The MRI can show hyperintensity of the renal parenchyma especially
at the cortical region and hypointensity at the medullary region. Also,
multiple hyperintense lesions in perirenal spaces on T2-weighted images
can be appreciated. Pediatric differential diagnosis includes polycystic
renal disease, urinoma, renal lymphoma with perirenal involvement, renal
tumors, etc. The diagnosis can be confirmed by needle aspiration of chylous
fluid or by renal biopsy but multi-modal imaging is characteristic.
Management is often conservative due to
the benign behavior of the lesion. Percutaneous drainage with administration
of intravenous albumin and enteral medium chain triglycerides may be indicated
if symptoms or ascites develop. Several cases of cyst decortication have
resulted in nephrectomy due to uncontrolled intraoperative bleeding. While
some suggest that asymptomatic patients with unchanged cystic lesions
on US do not require follow-up, we feel patients should undergo lifelong
follow-up as occasionally renal function will deteriorate.
REFERENCES
- Varela JR, Bargiela A, Requejo I, Fernandez R, Darriba M, Pombo F: Bilateral renal lymphangiomatosis: US and CT findings. Eur Radiol. 1998; 8: 230-1.
- Llorente JG, García AD, Sacristan JS, Chicharro GN: Renal lymphangiectasia: radiologic diagnosis and evolution. Abdom Imaging. 2002; 27: 637-9.
Fabian
Sanchez, Juan C. Prieto,
Korgun Koral & Linda A. Baker
Depart of Urology (FS, JCP, LAB) and
Radiology (KK)
Children’s Medical Center of Dallas
University of Texas Southwestern Medical Center
Dallas, Texas, USA
E-mail: Linda.baker@utsouthwestern.edu