TENSION-FREE
VAGINAL TAPE (TVT): MINIMALLY INVASIVE TECHNIQUE FOR STRESS URINARY INCONTINENCE
(SUI)
(
Download pdf )
PAULO C. R. PALMA, CÁSSIO L. Z. RICCETTO, MÍRIAM DAMBROS, VIVIANE HERRMANN, MARCELO THIEL, NELSON R. NETTO JR.
Department of Urology, Medical Sciences College, State University of Campinas (UNICAMP), Campinas, SP, Brazil
ABSTRACT
Objective:
The procedure o tension-free vaginal tape (TVT) was recently introduced
in the therapeutic armamentarium of stress urinary incontinence (SUI).
It is a pubovaginal sling applied in mid-urethra. The authors describe
their experience with this technique.
Materials and Methods: During the period
of May, 1999 to March, 2001, 110 patients (median age=53 years) were submitted
to TVT implant for the treatment of stress urinary incontinence. Clinical
exam and urodynamic studies were performed previously to surgery. All
patients referred symptoms consistent with stress incontinence, and 35.7%
complained of associated voiding urgency. Sixty-eight percent of the group
reported previous continence procedure. Urethral hypermobility was diagnosed
in 42% of patients (mean Valsalva leak point pressure under median effort
of 110 cmH2O), and 58% had intrinsic sphincter deficiency (mean Valsalva
leak point pressure under effort of 55 cmH2O).
Results: Mean patient follow-up was 18 months.
Ninety-two percent of the patients were submitted to anesthetic blockade
and 8% to local anesthesia. Mean length of the procedure was 30 minutes.
Dystopy correction, when present, was performed in the same procedure.
Mean hospital stay was 24 hours. There was bladder perforation in 13%
of cases of TVT. There was no urethral or vaginal erosion. Twenty patients
(18%) developed urgency symptoms during post-operative period, and 5 (4.5%)
presented urge incontinence. During this follow-up period, 81% remained
continent, 9% referred improvement of the symptoms compared to before
the procedure and 10% were not satisfied.
Conclusion: Our data allow us to conclude
that TVT procedure is safe, rapid and promoting adequate levels of continence
in mean term.
Key words:
urinary incontinence, stress; therapeutics; surgical procedures; prostheses
and implants
Int Braz J Urol. 2002; 28: 458-63
INTRODUCTION
The
use of autologous pubovaginal slings has been the preferred approach for
treating difficult cases of stress urinary incontinence (SUI) (1). This
preference to synthetic material occurs greatly because of two basic issues:
implant infection and urethral erosion (2).
On the other hand, the use of synthetic
slings transforms a complex surgery in a minimal invasive procedure, reducing
not only surgical time, as well as hospitalization period, post-operative
discomfort and time to recovery (1).
Recently, tension-free vaginal tape (TVT)
was introduced in therapeutic armamentarium, a synthetic sling applied
without tension, eliminating the issue of urethral erosion.
The paradigm’s change is not just in
eliminating the tension, which was already advocated by many authors,
but primarily placing the sling by vaginal route, in mid- or distal urethra,
instead of placing it in the bladder neck (3).
According to integral theory of continence
(4), pubourethral ligament together with pelvic floor muscles make distal
and midurethra the most important regions for urinary continence.
These new conceptions, associated to the
fact that sling surgeries are now widely used, makes TVT an alternative
for the surgical treatment of SUI.
The authors present their experience with
TVT for the surgical treatment of SUI.
MATERIALS AND METHODS
A prospective, randomized clinical trial
was performed with SUI patients. The project was approved by the Committee
of Ethics of the Hospital.
In the period of May, 1999 to March 2001,
110 patients with a diagnosis of SUI were submitted to TVT implant. Patients’
ages ranged from 42 to 72 years, median of 53 years. Patients were submitted
to clinical examination and urodynamic study previously to surgical procedure.
After the surgery the patients returned
monthly to the ambulatory for a clinical evaluation. In that moment they
were questioned about presence of spontaneous voiding, involuntary urinary
leakage, irritative bladder symptoms, vaginal and suprapubic pain, in
addition to questions about their satisfaction with the procedure.
In the absence of urinary leakage complaint
the patients were classified as continent. In the presence of this symptom,
the patients were grouped according to the severity of the leakage reported:
a)- More than 75% improvement from pre-operative symptoms; b)- 50-75%
improvement from pre-operative symptoms; c)- Less than 50% improvement;
d)- No alterations of the symptoms, or worsening, after the surgery.
In addition to the clinical history, we
proceeded to physical examination to evaluate the presence of urinary
leakage, signs of infection and erosion in vaginal wall.
In urodynamic study diagnosis of SUI due
to urethral hypermobility was made for patients presenting Valsalva Leak
Point Pressure (VLPP) above 90 cmH2O, and intrinsic sphincter deficiency
when VLPP was less than 90 cmH2O during urodynamic study (Table-1). Patients
presenting involuntary detrusor contractions during bladder filling, or
bladder outlet obstruction were excluded from the study.
In 35.7%, patients reported voiding urgency
associated to the symptoms of urinary leakage, and 68% reported history
of previous surgical procedure for the treatment of incontinence, the
most frequent procedure being Kelly-Kennedy surgery (86%).
At gynecological examination presence of
cistocele was verified in 34 patients (31%), and in 94% of the cases it
was grade I and in the remaining it was grade II. For 12 patients (11%)
rectocele was diagnosed e for 8 (7%) perineal rupture. For grade I cistoceles
repair was not performed; the procedure was executed in grade II cistoceles.
Dystopy correction was performed at the same surgical time during TVT
implant.
SURGICAL TECHNIQUE
The
procedure was performed with the patient in dorsal lithotomy position
and spinal anesthesia for the majority of the patients. One hundred and
one patients (92%) were submitted to spinal anesthesia and 9 (8%) to local
anesthesia and intravenous sedatives. In cases where it was necessary
to have surgical correction of dystopy, we choose, primarily, spinal anesthesia.
In cases where local anesthesia was used, the patient received intravenous
Midazolan™, 1mg before the procedure. For local anesthesia, we used
20mL 1% Marcain™ in 40mL of saline solution, and initially 5mL were
applied in skin and subcutaneous on each side, near the superior edge
of the pubic bone. Then, with a 22G spinal needle introduced near the
pubis in Retzius space, 15mL of the solution were applied bilaterally.
Vaginal anesthesia was performed by the injection of 20mL of anesthetic
solution on sub- and paraurethral regions, 1cm from urethral meatus, as
well as in vaginal pillars.
Two small 1cm transversal incisions were
performed near each side of the superior edge of the pubic bone to exteriorize
TVT trocar in this region. In the sequence, a median vaginal incision
of approximately 1.5cm was performed, initiating 1cm from urethral meatus
proximally, avoiding the bladder neck. Then, with a Metzenbaum scissor,
each side was bluntly dissected laterally, creating a 1cm tunnel, large
enough to introduce the tip of TVT trocar, which device was formed by
a polypropylene mesh covered by a plastic sheath, a curved trocar at each
end, a metallic introducer, and a straight metallic catheter guide to
introduce a Foley 20F catheter.
A Foley 20F catheter was introduced and
bladder was emptied and, in the sequence, with a metallic guide within
this catheter, the bladder was displaced away from the trocar. The sling,
that possesses a 5mm trocar at each end, was then prepared, introducing
one of these trocars in the introducer, and then guiding in the previous
dissected tunnels. Before the trocar, the catheter with the metallic guide
was lateralized in the same side where the trocar was introduced.
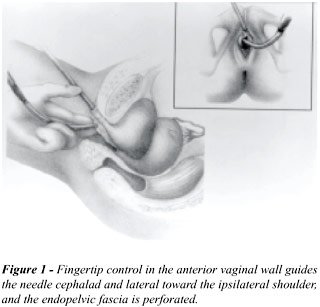
This trocar must be directed to the ipsilateral
shoulder of the patient, through two movements: in the first one, the
trocar must progress horizontally until it perforates endopelvic fascia
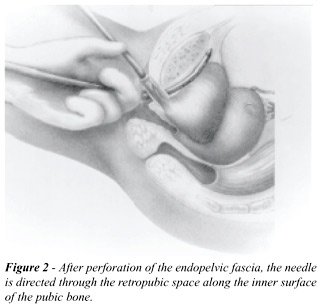
(Figure-1). The second movement consisted in a bascule movement, making
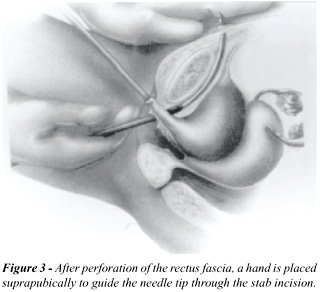
the trocar progress through the space of Retzius, tangent to pubis periosteum
until attaining suprapubic region, perforating rectus muscle and its fascia,
exteriorizing it through the incision previously performed (Figures-2
and 3).
The Foley catheter was removed and a cystoscopy
performed to assess possible bladder perforation. In case of perforation,
the trocar was removed and a new passage was made. Finally, the introducer
was removed and the trocar pulled, leading it to suprapubic region.
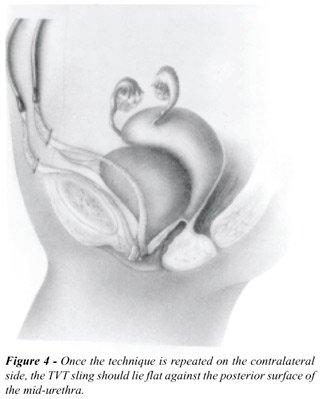
The same procedure was repeated on the contralateral
side, obtaining thus a U-loop of the pubovaginal sling in mid-urethra
(Figure-4).
The trocars were maintained in suprapubic
region and the adjustment of the tension was made before the removal of
the plastic sheaths (Figures-5 and 6). In patients submitted to local
anesthesia, the tape adjustment was made by the injection of 300mL saline
solution, asking the patient to cough vigorously and, in cases of presence
of urinary leakage, the ends of the sling were slightly pulled until continence
was observed. In cases where spinal anesthesia was used, intraoperative
adjustment of the tape was not performed.
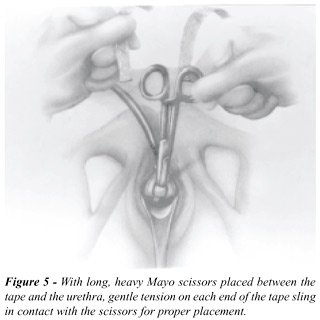
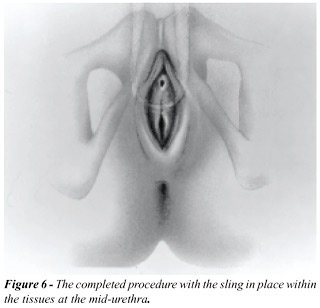
Before removing the plastics sheaths, a
scissor was placed between the TVT tape and the urethra. Then the TVT
ends were sectioned near to the skin, and suprapubic and vaginal incisions
were closed in standard fashion.
No indwelling catheter was left in place,
except for the cases of bladder perforation where the catheter was maintained
for 48 hours.
Antibiotics prophylaxis was made with sodium
cefalexine 1g 1h before the surgery and q6h until completing 24h.
RESULTS
Patients
mean follow-up was 18 months, range from 2 to 24 months. Mean length of
procedure was 30 minutes, range from 20 minutes to 1h30min. In cases of
dystopy correction, surgical time increased approximately 40 minutes.
Mean hospital stay was 24 hours (range from 12 to 36 hrs). Inadvertent
bladder perforation, in its superolateral wall, occurred in 14 patients
(13%), which maintained bladder catheter for 48 hours, with no further
complications. Post-operative urinary retention occurred in 10 patients
(9%), among these 9 (90%) voided spontaneously in up to 14 days from the
surgical procedure. These patients were treated with bladder catheter
in the first 7 days and, then, with clean intermittent catheterization
until resolution of the urinary retention. In one patient a surgical lyses
of one side of the TVT was required 2 months after the implant, due to
persistent retention, and she has progressed without retention and continent.
No vaginal wall infection neither tape erosion
for the urethra or vagina was observed. Irritative post-voiding symptoms
were reported by 32 patients (29%) during early post-operative period
(until 4 weeks after the surgery), 20 (18%) maintained urgency symptoms,
and 5 (4.5%) had urge incontinence complaints sustained. This group of
patients was submitted to a new urodynamic evaluation, evidencing detrusor
instability in 38 patients (35%), urinary incontinence with VLPP less
than 60 mmH2O in 33 (30%), and absence of significant alterations on the
remainder. Patients with detrusor instability were followed and treated
with oral anticholinergic agents. No case required the removal of TVT
due to failure of drug therapy.
Until the follow-up described, we observed
that 89 patients (81%) were continent, 10 (9%) reported improvement over
75% and 11 (10%) were unsatisfied with the procedure.
DISCUSSION
There
is a consensus in recent studies that pubovaginal sling and retropubic
urethrocystopexy are the therapeutic techniques of stress urinary incontinence
offering the best continence results after long term follow-up (1). However,
slings imply a considerable time of surgical training, presenting the
inconvenience of requiring a donator region for harvesting the fascia
to be used, besides the risk of bladder outlet obstruction and other bladder
dysfunctions (3). On the other hand, retropubic urethrocystopexy imply
performing an abdominal incision, with increases in morbidity and hospital
stay and, when performed by laparoscopy, promotes important cost elevation,
in addition to the required learning curve (4). Thus, the need for the
development of minimal invasive techniques is warranted.
TVT corresponds conceptually to a sling
and, thus, promotes an increase of urethral resistance because of the
creation of a suburethral support zone, avoiding rotational and descending
urethral movement, when elevation of abdominal pressure occurs. In addition,
if facilitates the coaptation of urethral lumen at rest and with straining.
However, contrarily to classical pubovaginal slings, TVT is applied in
mid-urethra, where pubourethral ligaments are inserted, responsible for
natural stabilization of the urethra (5). Maintenance of the tape in an
adequate position may be explained by its saliencies and indentations,
and by the “nipping” effect of pelvic fascias and rectus muscle,
and of local inflammatory reaction (6,7).
Until today, no specific problems were described
to this technique, but blood dyscrasia is considered a contraindication
because retropubic space dissection is performed without direct vision,
and there is risk of vascular lesion. Thus, as in other techniques for
treating SUI and, specially, because it deals with synthetic material,
a careful vaginal antisepsis is required, as well as excluding urinary
tract infections and vulvovaginitis. Although in our study there is a
predominance of patients with previous continence surgeries for stress
urinary incontinence, no significant complications or difficulties were
observed during the surgery. Contrarily to that previously described with
the use of synthetic sling (2), no rejection of the implanted material
was observed. This may be due by the minimally invasiveness of the procedure,
associated to a small surgical time and the use of prophylactic antibiotics
before the surgery.
Although our series does not show post-operative
urodynamic evaluation, we may suppose that this technique does not alter
voiding pressure, as it happens with periurethral injections. TVT is applied
without tension and does not limit bladder neck opening, as conventional
slings do (7). Though our series present 9% of urinary retention, this
may be due to spinal anesthesia used in 90% of patients, and have no direct
relation to the surgical technique used. We have chosen spinal anesthesia
because we are in an faculty service where resident doctors are trained,
and that makes patient manipulation easiest, bringing as minimal discomfort
as possible.
Consistency with physiological principles
of urinary continence in women, and cure rates above 80% in 2 years mean
follow-up (8,9) warrant stating that this procedure is a promising progress
in SUI surgical treatment. This is a less invasive surgery that may be
performed on an ambulatory basis and with good cost-benefit profile.
CONCLUSION
TVT is a minimal invasive surgical procedure for the treatment of stress urinary incontinence. Although a recent and costly procedure for the majority of our patients, it has been presenting satisfactory and lasting results that encourage its use in surgical practice.
REFERENCES
- Norris JP, Breslin DS, Staskin DR: Use of synthetic material in sling surgery: a minimally invasive approach. J Endourol. 1996; 10: 227-30.
- Palma PCR, Ikari O, D’Ancona CAL, Netto NR Jr: Alça pubovaginal sintética no tratamento da incontinência urinária de esforço. J Bras Urol. 1992; 18: 202-4.
- Ulmsten U, Henriksson L, Johnson P, Varhos G: An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J. 1996; 7: 81-6.
- Petros P, Ulmsten U: An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J urol Nephrol. 1993; 153: 1-93.
- Ulmstem U, Falconer C, Johnson P, Jomaa M, Lannér L, Nilsson CG, et al.: A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J. 1998; 9: 210-13.
- Carlin BI, Klutke JJ, Klutke CG: The tension-free vaginal tape procedure for the treatment of stress incontinence in the female patient. Urology 2000; 5 (6 Suppl): 28-31.
- Klutke JJ, Carlin BI, Klutke CG: The tension-free vaginal procedure: correction of stress incontinence with minimal alteration in proximal urethral mobility. Urology 2000, 55: 512-4.
- Jimenez CJ, Hualde AA, De Garibay ASG, Uruñuela FL, Cárdenas AP, Paul MP, et al.: TVT (tension-free tape). New surgical technique in the treatment of stress urinary incontinence. Arch Esp Urol. 2000; 53: 9-13.
- Wang AC, Lo TS: Tension-free vaginal tape. A minimally invasive solution to stress urinary incontinence. J Reprod Med. 1998; 43: 429-34.
_______________________
Received: January 22, 2002
Accepted after revision: August 5, 2002
_______________________
Correspondence address:
Dr. Míriam Dambros
Rua Engenheiro Edward de Vita Godoy, 966 / 12
Cidade Universitária, Distrito de Barão Geraldo,
Campinas, SP, 13084-090, Brazil
E-mail: miriamdambros@hotmail.com