SEXUAL
REHABILITATION AFTER RADICAL RETROPUBIC PROSTATECTOMY: NEW TECHNIQUE USING
ILIO-INGUINAL NERVE GRAFT
(
Download pdf )
MIGUEL SROUGI, DANIEL PEREIRA, MARCOS DALL‘OGLIO
Division of Urology, Paulista School of Medicine, Federal University of São Paulo (UNIFESP), São Paulo, SP, Brazil
ABSTRACT
Sural
nerve grafts have been used to repair the cavernous nerves and allow sexual
potency recovery after radical prostatectomy. In order to overcome the
drawbacks related to the harvesting of the sural nerve, the authors developed
an original technique using ilio-inguinal nerve grafts to repair the cavernous
innervation during radical prostatectomy.
This technique used in a group of new patients
proved its feasibility and absence of intra- and postoperative complications.
Compared to sural nerve the use of ilio-inguinal graft has some advantages:
1)- Greater familiarity for urologists to harvest the ilio-inguinal nerve;
2)- Less time to acquire the graft; 3)- Greater postoperative comfort,
avoiding inferior limb pain and edema, that delay patients’ mobilization
and recovery; 4)- Absence of anesthesia or paresthesia in the calcaneal
area; 5)- Absence of sympathetic reflex dystrophy in inferior limbs.
Key words:
prostate; prostatectomy; penile erection; inguinal canal; nerve transfer;
sural nerve
Int Braz J Urol. 2002; 28: 446-51
INTRODUCTION
Progress
in radical retropubic prostatectomy technique popularized and made this
procedure less aggressive to the patients (1,2). Considering that highly
satisfactory rates of cure are obtained with this method efforts are still
needed in order to decrease the morbidity of the procedure, mainly urinary
incontinence, and erectile dysfunction (3,4).
The ability to maintain spontaneous erection
after radical retropubic prostatectomy is directly linked to preservation
of the autonomous innervation (5). Cavernous nerve is represented by a
gathering of parasympathetic nerve fibers included in the neurovascular
bundle that runs along the lateral-posterior aspect of the prostate. In
1984, Walsh (6) described the cavernous nerve-sparing technique in radical
retropubic prostatectomy that reduced, but did not eliminate the risk
of erectile dysfunction. Other authors applied the surgical principles
of Walsh and were able to preserve the sexual function following radical
retropubic prostatectomy in 30% to 60% of the cases (7,8).
After experimental tests in rats, autologous
nerve transplant was proposed with the aim to circumvent lesions of the
cavernous neurovascular bundles (9,10). Kim et al. (11-13) began to use
in the clinical setting sural nerve grafts to replace injured cavernous
nerves, making possible the recovery of erectile function in 43% of patients
who had both cavernous bundles resected.
In spite of its proven clinical efficiency
as graft material, the use of sural nerve has some drawbacks both to specialists
and to patients. The sural nerve area is not familiar to the urologist
and local interventions require the creation of a second surgical field,
increasing the operative time. Furthermore, appropriate equipment, and
anatomic and technique specific knowledge, are necessary to the extraction
of this nerve (11,12). Besides these problems, the removal of this nerve
can be followed by some complications, such as paresthesia in the lateral
surface of the foot, local hematomas, chronic pain in leg, delay in patients
postoperative deambulation, greater risk of surgical infection and sympathetic
reflex dystrophy (12).
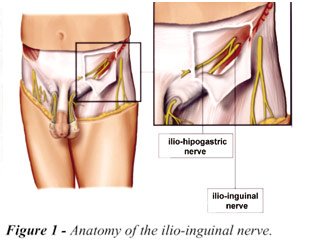
For these reasons, we devised an alternative
for performing nervous grafts to replace cavernous nerves. During inguinal
herniorraphy or high orchiectomy, we use to identify and isolate the ilio-inguinal
nerve, that originates in L1 root and at anterior abdominal wall level
is located between internal and external oblique muscles, lying distally
over the spermatic cord (14). In order to avoid postoperative pain due
to accidental inclusion of this nerve in the abdominal wall reinforcement
sutures, we used to perform routinely its resection, without seen any
morbidity associated with its extraction. This nerve, until then despised,
could be a valuable element to cavernous nerves reconstruction.
Although we could not find previous studies
regarding the use of ilio-inguinal nerves for grafting we decided to explore
its use as graft material for cavernous nerve replacement, trying to overcome
the problems caused by sural nerve harvesting (12).
SURGICAL TECHNIQUE
Before
performing the infra-umbilical incision for radical retropubic prostatectomy,
we proceed with the removal of the left ilio-inguinal nerve through an
oblique incision of about 3 cm in the lower left abdominal quadrant, at
the cutaneous projection of the external inguinal ring (Figures-1 and
2). The incision is deepened until reaching the external oblique muscle
aponeurosis that is also obliquely incised, from the external inguinal
ring for about 6 cm cranially. After opening this aponeurosis, one can
identify the ilio-inguinal nerve, which is dissected in cranial and caudal
direction (Figure-1). For grafting purpose we try to remove when possible
a nerve segment of about 12 cm, that allows for making 2 grafts with 5
to 6 cm each. (Figure-2B).
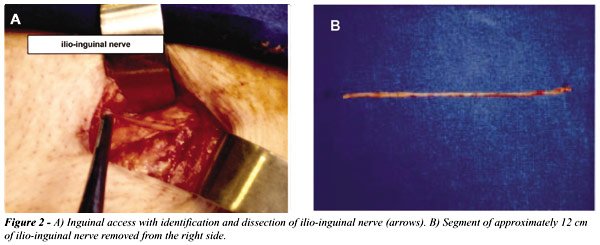
The resected nerve segment is kept in saline
solution with gentamycin (80 mg/L) until the placement of the graft, and
the lateral abdominal wall incision is closed by layers, successively,
external oblique muscle aponeurosis, subcutaneous, and skin. After the
removal of the graft, radical retropubic prostatectomy is initiated using
the modified Walsh technique (15).
After completing the removal of the prostate
and closing the bladder neck, and before performing vesicourethral anastomosis,
unilateral or bilateral ilio-inguinal graft is done. To be accomplished
successfully it is necessary to have a bloodless field, which is obtained
with careful hemostasia of the periprostatic area. An ilio-inguinal nerve
segment of 5 to 6 cm is placed over the cavernous bundle course in one
or in both sides and the graft is performed by suturing its extremities
to the transected surfaces of the cavernous nerve, located distally in
the dorsolateral periurethral area and proximally in the dorsolateral
perivesical region (Figure-3). The nerve grafting must be performed without
tension, with one interrupted prolene 6-0 sutures applied in each extremity,
under 4x loupe magnification. In our first cases, we used three sutures
at each end but we moved to a single stitch in the more recent cases in
order to decrease local foreign body reaction. It should be emphasized
that the nerve segment must be 10% to 20% longer than the created defect,
so that it compensates subsequent graft shrinkage (11).
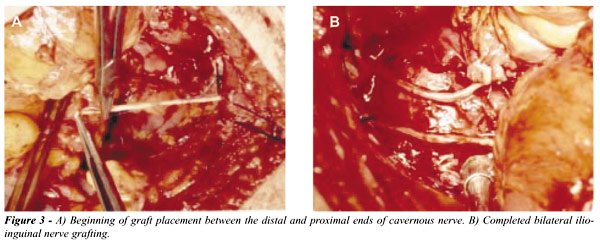
With the anastomosis of both sides completed
and the local hemostasia reviewed, radical prostatectomy is concluded
through the vesicourethral anastomosis and local draining.
COMMENTS
In
this present study, we presented an original technique for restoration
of the cavernous innervation during radical retropubic prostatectomy,
using ilio-inguinal nerve instead of sural nerve graft recommended by
other authors (12).
Nervous grafts are a well-established method
for injury repair of motor, sensitive, and autonomous nerves (16). The
graft works as a conduit that directs the nervous fibers regeneration
between the injured extremities, avoiding fibrosis and neuroma.
Between January and May 2002, 39 patients
were submitted to the procedure in our facility, including 17 bilateral
and 22 unilateral grafts. With this experience we did confirm some advantages
of this new technique: 1) Negligible increase of the total surgical time,
about 10-15 minutes for the acquisition and 10 minutes for the placement
of the grafts; 2) The entire procedure is performed at the same surgical
field; 3) Surgical access is familiar to urologists; 4) Easy and efficient
inguinal hemostasia; 5) Special instruments are not necessary, such as
nerve extractor. Furthermore, the ilio-inguinal graft can be performed
without significant surgical complications. It is well known that the
use of the sural nerve as a graft material can be followed by complications
that sometimes are not negligible (11,12).These patients have higher incidence
of local infection, since the procedure involves inferior limbs manipulation
in usually older individuals. Also, almost all patients complain of anesthesia
of the lateral side of the foot, which increases the risks of local accidental
wounds. The presence of local pain and edema, common in these cases, can
impair early deambulation and postoperative recovery and, in some patients,
sural nerve resection can lead to sympathetic reflex dystrophy, with pain,
motor alterations and distal muscular atrophy of the limb.
On the contrary, none of the 39 patients
treated with our technique presented infection, pain, nor local sensibility
changes after the intervention. The sole inconvenient for the use of ilio-inguinal
nerve is that sometimes its caliber is much reduced, making impossible
its utilization. This occurred in 1 of 40 attempts (2,5%), which shows
that this phenomenon is actual, but very uncommon. It is worth reminding
that ilio-inguinal resection has low neurologic morbidity, for its sensitive
innervation areas, which include the pubis region, penis root and superior-lateral
surface of the thigh, are also supplied by communicating branches of the
genito-femoral and ilio-hypogastric nerves (14).
The early clinical studies reported by Kim
et al. (11,12) with the use of sural nerve graft proved the feasibility
of the method. A more recent paper from this group, analyzing extended
follow-up of 23 patients submitted to the procedure after bilateral excision
of the cavernous bundles, showed total or partial penile erection recovery
in 56% of the cases (13). Ten of the 23 patients (43%) were able to engage
in full sexual activity with the aid of sildenafil, and in all cases erections
only returned after 5 months from the intervention.
In our group of treated patients, the efficiency
of the procedure still cannot be evaluated, due to the limited time of
postoperative follow-up and also because in many of these patients one
of the cavernous bundles was preserved. Furthermore, in some of our cases
the graft was applied in parallel, with the aim of increase the chances
for sexual recovery. Considering the available favorable data from the
literature, it is possible that the rates of sexual dysfunction will be
reduced in our patients. Future evaluations of the patients that were
submitted to bilateral grafting after removal of both cavernous nerves
will prove the real value of the ilio-inguinal graft technique in the
sexual rehabilitation after radical prostatectomy.
REFERENCES
- Walsh PC, Lepor H, Eggleston JC: Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate. 1983; 4: 473-85.
- Davidson PJ, Van den Ouden D, Schroeder FH: Radical prostatectomy: prospective assessment of mortality and morbility. Eur Urol. 1996; 29: 168-73.
- Eastham J, Kattan MW, Rogers E, Goad JR, Ohori M, Boone TB, et al.: Risk factors for urinary incontinence after radical prostatectomy. J Urol. 1996; 156: 1707-13.
- Schover LR: Sexual rehabilitation after treatment for prostate cancer. Cancer. 1993; 71(Suppl. 3): 1024-30.
- Breza J, Aboseif SR, Orvis BR, Lue TF, Tanagho EA: Detailed anatomy of penile neurovascular structures: surgical significance. J Urol. 1989; 141: 437-43.
- Walsh PC, Epstein JI, Lowe FC: Potency following radical prostatectomy with wide unilateral excision of the neurovascular bundles. J Urol. 1987; 138: 823-7.
- Bigg SW, Kavoussi LR, Catalona WJ: Role of nerve-sparing radical prostatectomy for clinical stage B2 prostate cancer. J Urol. 1990; 144: 1420.
- Geary ES, Dendinger TE, Freiha FS, Stamey TA: Nerve sparing radical prostatectomy: a different view. J Urol. 1995; 154: 145-9.
- Ball RA, Lipton SA, Dreyer EB, Richie JP, Vickers MA: Entubulization repair of severed cavernous nerves in the rat resulting in return of erectile function. J Urol. 1992; 148: 211-5.
- Quinlan DM, Nelson RJ, Walsh PC: Cavernous nerve graft restore erectile function in denervated rats. J Urol. 1991; 145: 380-3.
- Kim ED, Scardino PT, Hampel O, Mills NL, Wheeler TM, Nath RK: Interposition of sural nerve restores function of cavernous nerve resected during prostatectomy. J Urol. 1999; 161: 188-92.
- Kim ED, Seo JT: A minimally invasive technique for sural nerve harvesting. Urology. 2001; 57: 921-4.
- Kim ED, Nath R, Slawin KM, Kadmon D, Miles BJ, Scardino PT: Bilateral nerve grafting during radical retropubic prostatectomy: extended follow up. Urology. 2001; 58: 983-7.
- Nahabedian MY, Dellon AL: Outcome of operative management of nerve injuries in the ílioinguinal region. J Amer Coll Surg. 1997; 184: 265-8.
- Srougi, M.: Radical Prostatectomy with Preservation of Erectile Function. In: Srougi M, Simon SD (eds.), Urological Cancer. São Paulo, Platina, 1995, pp 361-376, [in Portuguese].
- Sunderland S: Nerve Grafting and Related Methods of Nerve Repair. In: Sunderland S (ed.), Nerve Injuries and Their Repair: a Critical Appraisal. New York, Churchill Livingstone, 1991, pp 467-497.
____________________
Received: May 15, 2002
Accepted after revision: July 20, 2002
_______________________
Correspondence address:
Dr. Miguel Srougi
Rua Ministro Rocha Azevedo, 1388 / 61
01410-002, São Paulo, SP, Brazil
Fax: + 55 11 287-2821
E-mail: srougi@attglobal.net
EDITORIAL COMMENT
The
technique of interposition nerve grafting during radical prostatectomy
(RP) has generated considerable interest over the last 5 years. This procedure
enables a select group of men the ability to maintain spontaneous erections,
even after resection of both neurovascular bundles (NVBs). The most recent
data from the Baylor College of Medicine, USA, demonstrates a 43% Viagraä
potency rate with 2 year follow-up in a group of 23 men undergoing bilateral
graft placement after bilateral NVB resection (Kim ED, et al.: Urology
2001; 58:9837). Wood et al. from the M.D. Anderson Cancer Center in Houston,
Texas, USA, provided important confirmation of our results by demonstrating
nearly identical results in 30 men (Wood CG, et al.: J Urol. 2002; 167:157,
Abst. 629, AUA Annual Meeting, Orlando FL, May 2002).
Urologists have been hesitant to use the
sural nerve because of lack of familiarity with this peripheral sensory
nerve. Difficulties in scheduling operative time with a plastic or neurosurgeon
familiar with harvesting techniques further complicates the procedure.
In an effort to overcome these issues, Srougi et al. have presented a
new technique using the ilio-inguinal nerve as the graft template. They
report that the procedure is feasible and without significant morbidity.
If their results regarding return of potency are favorable, then use of
the ilio-inguinal nerve may certainly increase the popularity of interposition
grafting during RP.
In the early 1990s, Dr. Patrick Walsh from
Baltimore, Maryland, USA, was the first to perform nerve grafting during
RP. One of our concerns with his methodology was the use of the genitofemoral
nerve given its very small caliber compared with the sural nerve. The
sural nerve is comparable to the obturator nerve in size, several folds
larger in caliber than the genitofemoral or ilio-inguinal nerve. These
larger caliber nerve grafts probably have an increased likelihood of neural
regeneration and graft take. The NVB plexus is wider than the sural nerve,
and certainly more than the ilio-inguinal nerve. Use of the ilio-inguinal
nerve for grafting purposes is extremely uncommon in nerve grafting circles.
The sural nerve was selected because 1)- it is the standard used for most
nerve grafting procedures, 2)- its large size is beneficial for nerve
regeneration, 3)- it is easily harvested with minimal training, and 4)-
the morbidity associated with its harvest has been extremely low. In my
experience, patients are only minimally bothered by the numbness on the
side of the foot and ambulation has not been delayed. I am not aware of
the development of reflex sympathetic dystrophy in the estimated more
than 400 procedures performed at various centers in the United States
to date, although this complication may occur with the division of any
nerve.
Dr. Srougi’s work represents an important
and welcome step in the development of any procedure - that is, attempts
at improvements in technique. For example, several European urologists
have performed laparoscopic nerve grafts during RP. Undoubtedly, some
innovative researcher will develop a “quick connect” method
to simplify the anastomosis. We will all be eagerly anticipating the potency
outcome of Dr. Srougi’s 39 men over the next several years. If it
works, I would certainly be interested in trying it!
Dr. Edward D. Kim
Associate Professor of Surgery
University of Tennessee
Knoxville, Tennessee, USA