PATIENT
POSITION AND SEMI-RIGID URETEROSCOPY OUTCOMES
( Download
pdf )
FERNANDO KORKES, ANTONIO C. LOPES-NETO, MARIO H. E. MATTOS, ANTONIO C. L. POMPEO, ERIC R. WROCLAWSKI
Division of Urology, ABC Medical School, Santo Andre, Sao Paulo, Brazil
ABSTRACT
Introduction:
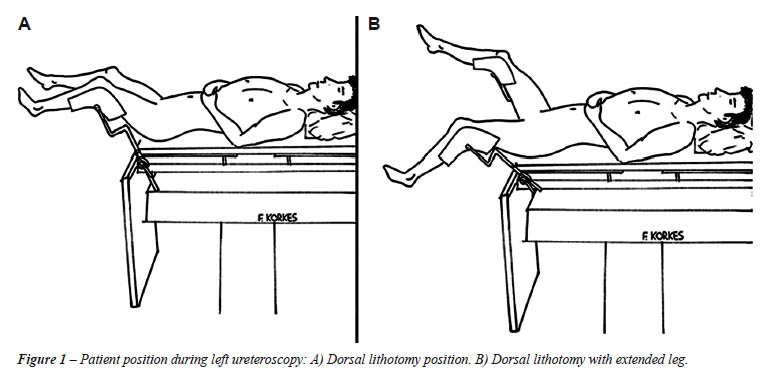
Two positions have been reported for ureteroscopy (URS): dorsal lithotomy
(DL) position and dorsal lithotomy position with same side leg slightly
extended (DLEL). The aim of the present study was to compare the outcomes
associated with URS performed with patients in DL vs. DLEL position.
Materials and Methods: A total of 98 patients
treated for ureteral calculi were randomized to either DL or DLEL position
during URS, and were prospectively followed. Patients, stone characteristics
and operative outcomes were evaluated.
Results: Of the 98 patients included in
the study, 56.1% were men and 43.9% women with a mean age of 42.6 ±
16.8 years. Forty-eight patients underwent URS in DL position and 50 in
DLEL position. Patients’ age, mean stone size and location were
similar between both groups. Operative time was longer for the DL vs.
DLEL group (81.0 vs. 62.0 minutes, p = 0.045), mainly for men (95.2 vs.
63.9 minutes, p = 0.023). Mean fluoroscopy use, complications and success
rates were similar between both groups.
Conclusions: Most factors associated with
operative outcomes during URS are inherent to patient’s condition
or devices available at each center, and therefore cannot be changed.
However, leg position is a simple factor that can easily be changed, and
directly affects operative time during URS. Even though success and complication
rates are not related to position, placing the patient in dorsal lithotomy
position with an extended leg seems to make the surgery easier and faster.
Key
words: ureteroscopy; ureteral calculi; lithotripsy; prospective
studies; lithiasis; urinary catheterization
Int Braz J Urol. 2009; 35: 542-50
INTRODUCTION
Ureteroscopy
(URS) has gained widespread use for the treatment of ureteral stones (1,2).
For most endoscopic procedures, patients are placed in the standard dorsal
lithotomy position and the perineum flush with the end of the cystoscopy
table. Two positions have been reported for URS procedures: dorsal lithotomy
position with legs supported in stirrups with minimal flex at the hips
(DL) (3,4); and dorsal lithotomy position with one leg (same side of ureteral
stone) slightly extended, and the hip abducted (DLEL) (5) (Figure-1).
This position has the theoretical advantage of minimizing the angulation
of the ureter, facilitating passage and advancement of the ureteroscope
(6,7).
However, different groups have adopted
both positions, and after video cameras had been selected for such procedures,
many surgeons have subsequently used the DL position. To our knowledge,
no studies have assessed the differences between these two approaches.
The aim of the present study was to compare the outcomes associated with
URS performed with patients in DL vs. DLEL position, significant operative
time, stone free and complication rates. As secondary outcomes, fluoroscopy
time, need for ureteral dilatation, use of ureteral stents and length
of hospital stay was also assessed.
MATERIALS AND METHODS
A
total of 98 patients treated for ureteral calculi at a single institution
from January 2004 to January 2008 were randomized to either DL or DLEL
position during URS, and were prospectively followed. All patients were
operated by second-year-residents-in-training, under supervision of the
same urologist (ACLN), always as first assistant (total of eight residents).
The ureteroscope (7.5F rigid ureteroscope, Karl Storz, Germany), fluoroscopy,
video monitor, baskets and irrigation devices were the same for both groups.
Balloon ureteral dilatation was performed in selected cases for technical
difficulties, and ureteral assess was always obtained after passing two
guide wires. Lithotripsy was performed with pneumatic lithotripter (Swiss
Lithoclast, Electro Medical Systems, Switzerland) under general or regional
anesthesia. A 6F or 7F ureteral stent was inserted at the end of the procedure
according to surgeon’s judgment.
Patients and stone characteristics and operative
outcomes were evaluated. Patients included in the study had ureteral calculi
to be treated surgically. Exclusion criteria included the presence of
infection, inadequate follow-up or hip limitations. Two patients were
excluded from the study. Main outcomes to be assessed included operative
time, fluoroscopy time, intra-operative complications, postoperative complications,
stone free rate, use of ureteral stents and length of hospital stay. Primary
end-point was to leave the patient stone free with minimal morbidity,
in a short period of time and with low radiation exposition. Statistical
analysis was performed using the Statistical Package for Social Sciences
software (SPSS 13.0 for Mac OS X, SPSS, Inc., Chicago, IL. USA). Student’s-t
test-was used to compare means and chi-square to compare categorical outcome
variables. Statistical significance was determined at p value less than
0.05. All patients or parents/tutors signed an informed consent form,
and the institutional review board approved the present study.
RESULTS
Of
the 98 patients included in the study, 55 (56.1%) were men and 43 (43.9%)
women with a mean age of 42.6 ± 16.8 years (range 9 - 84 years).
Forty-eight patients underwent URS in DL position and 50 in DLEL position.
Patients’ age, mean stone size and location were similar between
both groups (Table-1).
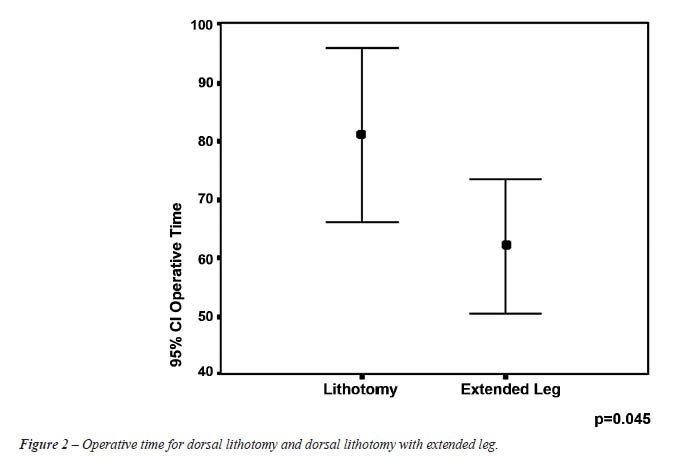
Operative outcomes for both groups are shown in Table-2. Operative time
was longer for the DL vs. DLEL group (81.0 vs. 62.0 minutes, p = 0.045,
Figure-2). Mean fluoroscopy use, complications and success rates were
similar between both groups (Table-2). If men vs. women were compared
in both groups, operative time was 95.2 vs. 64.5 minutes (p = 0.036) for
DL and 63.9 vs. 59.5 minutes (p = 0.709) for DLEL. If DL men vs. DLEL
men were compared, there was also a significant difference (p = 0.023),
which did not occur between DL women vs. DLEL women (p = 0.668).
The intra-operative complication rate was 3.1%, similar between both groups (p = 0.371), with medical vs. surgical complications accounting for 1.0 vs. 2.1%. Complications included one case of bronchospasm requiring tracheal intubation and 2 cases that required open conversion (one for ureteral damage while treating a large proximal stone in the DL group and one in DLEL group due to failure to access a large proximal stone). Minor complications occurred in 13.3% of the patients and included minor mucosal damage (9.2%), equipment malfunction (3.1%) and failure to place the ureteral stent (1.0%).
COMMENTS
Intracorporeal
lithotripsy technology has made it possible to successfully access and
treat virtually any stone within the upper urinary tract (1,8). Operative
outcomes have been associated with several factors, such as stone size,
stone location, energy source for lithotripsy, balloon dilatation, duration
of stone disease, surgeon’s experience, etc. (1,9-13). Most of these
factors are inherent to patient’s condition or devices available
at each center, and therefore cannot be changed. However, leg position
is a simple factor that directly affects ureteral access and kinking and
can easily be changed (7).
Different leg positions have been used
during URS procedures. The position of the patient with the same side
leg lower and medially positioned and with the other leg higher and more
laterally positioned has the theoretical advantage of straightening the
ureteral angle. Angus et al. have demonstrated in a radiographic study
that the ureteral angle at the iliac vessels level straightens according
to patient position, even though it does not interfere with the intramural
portion of the ureter (7). However, other factors might also interfere
such as the angle between the urethra/bladder neck and the ureteral orifice.
It is noteworthy that the role of patient’s position in URS outcomes
has never, to our knowledge, been previously evaluated, and clinical studies
are necessary to validate this experimental study. In fact, several studies
that evaluate URS outcomes do not in fact mention which position patients
were placed during procedures (1,10,14).
Our study has some important findings.
First, we have observed longer operative time when patients were in DL
vs. DLEL position. Different authors have used different leg positions
during URS (3-6), and according to our study, this detail directly affects
the operative time. This observation might reflect an increased difficulty
both to access the ureter and also that kinking in the ureter produces
to stone fragmentation and removal, subsequently taking a longer time
to access the ureter. Therefore, the theoretical support for the DLEL
position might be correct. Since this observation, our group has adopted
the DLEL as the standard position for URS. DLEL might not only straighten
the ureter to be assessed, but also with the flexed leg, the surgeon and
the assistant have a better working space.
Second, this difference was even more important
when operating men, resulting in a significant decrease in operative time
with DLEL position (p = 0.02). For men, the extended leg might bring an
additional benefit of straightening and aligning the urethra, which did
not occur in women (p = 0.668).
Third, complication and success rates were
similar for DL vs. DLEL groups, and both positions are feasible. Although
surgery might be easier and faster when patients are positioned in DLEL,
if for any reason the patient is positioned in DL, surgical outcomes are
expected to be the same. If there are limitations regarding cystoscopy
table positioning, URS can still be performed safely.
Our study has some limitations. First,
this was not a blinded study, as the surgeon was aware of leg position.
Nevertheless, we believe that this bias does not seem to affect surgical
procedures. Further studies evaluating the length of time spent in each
stage of surgery (bladder access, ureteral access, lithotripsy, ureteral
stenting) as well as subjective impression of the level of difficulty
according to patient position could produce additional information. Moreover,
other important factors such as stone composition were not evaluated in
the present study. However, this limitation is the same as in a clinical
setting when this information cannot be obtained preoperatively. Moreover,
as previously stated, stone composition is another factor that cannot
be modified preoperatively, differently from leg position.
Complication and ureteral stenting rates
were also slightly higher than in larger series. Possible reasons for
these findings include the facts that these patients were operated by
residents-in-training and as this population of patients have a great
difficulty in fixing an appointment with the urologist, as we primarily
treat large (mean size 9.9 mm) and chronic (mean history time of 148 days)
ureteral calculi. In this subset of patients, more complications are expected
(15), and ureteral stenting can be beneficial (16). One case required
open conversion due to ureteral avulsion while treating a large proximal
stone, a rare complication of this procedure (this was the only event
in our series of more than 900 ureteroscopies performed); the other patient
had a 12 mm proximal stone that could not be reached with the ureteroscope.
As we do not have a flexible ureteroscope or a flexible nephroscope, our
option was to convert to an open surgery and remove the stone, with an
unremarkable postoperative evolution.
In conclusion, patient position during
URS directly affects operative time. Even though success and complication
rates are not related to position, placing the patient in dorsal lithotomy
position with an extended leg seems to make the surgery easier and faster,
specially when operating males.
CONFLICT OF INTEREST
None declared.
REFERENCES
- Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al.: 2007 guideline for the management of ureteral calculi. J Urol. 2007; 178: 2418-34.
- Rofeim O, Yohannes P, Badlani GH: Does laparoscopic ureterolithotomy replace shock-wave lithotripsy or ureteroscopy for ureteral stones? Curr Opin Urol. 2001; 11: 287-91.
- Ziaee SA, Halimiasl P, Aminsharifi A, Shafi H, Beigi FM, Basiri A: Management of 10-15-mm proximal ureteral stones: ureteroscopy or extracorporeal shockwave lithotripsy? Urology. 2008; 71: 28-31.
- Watterson JD, Girvan AR, Beiko DT, Nott L, Wollin TA, Razvi H, et al.: Ureteroscopy and holmium:YAG laser lithotripsy: an emerging definitive management strategy for symptomatic ureteral calculi in pregnancy. Urology. 2002; 60: 383-7.
- Lopes Neto AC, Gava MM, Mattos MHE, Borreli M, Wroclawski ER: Treatment of ureteral calculi by ureteroscopy: experience of 100 cases at the Faculdade de Medicina do ABC (FMABC – Medical School). Einstein. 2004; 2: 28-32.
- Su LM, Sosa ES: Ureteroscopy and Retrograde Ureteral Access. In: Walsh PC (ed.), Campbell’s Urology. Philadelphia, Saunders, 2002; pp. 3314.
- Angus DG, Webb DR: Influence of hip flexion on the course of the ureter. Ureteroscopic implications. Eur Urol. 1988; 14: 287-90.
- Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck AC, Gallucci M, et al.: 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007; 52: 1610-31.
- Al-Awadi K, Kehinde EO, Al-Hunayan A, Al-Khayat A: Iatrogenic ureteric injuries: incidence, aetiological factors and the effect of early management on subsequent outcome. Int Urol Nephrol. 2005; 37: 235-41.
- Leijte JA, Oddens JR, Lock TM: Holmium laser lithotripsy for ureteral calculi: predictive factors for complications and success. J Endourol. 2008; 22: 257-60.
- Korkes F, Gomes SA, Heilberg IP: Diagnosis and treatment of ureteral calculi. J Bras Nefrol. 2009; 31: 55-61.
- Natalin R, Xavier K, Okeke Z and Gupta M: Impact of obesity on ureteroscopic laser lithotripsy of urinary tract calculi. Int Braz J Urol. 35: 36-41; discussion 41-2, 2009.
- Fuganti PE, Pires SR, Branco RO and Porto JL: Ballistic ureteroscopic lithotripsy in prepubertal patients: a feasible option for ureteral stones. Int Braz J Urol. 32: 322-7; discussion 327-9, 2006.
- Mugiya S, Ozono S, Nagata M, Takayama T, Nagae H: Retrograde endoscopic management of ureteral stones more than 2 cm in size. Urology. 2006; 67: 1164-8; discussion 1168.
- Brito AH, Mitre AI, Srougi M: Ureteroscopic pneumatic lithotripsy of impacted ureteral calculi. Int Braz J Urol. 2006; 32: 295-9.
- Hao P, Li W, Song C, Yan J, Song B, Li L: Clinical evaluation of double-pigtail stent in patients with upper urinary tract diseases: report of 2685 cases. J Endourol. 2008; 22: 65-70.
____________________
Accepted after revision:
June 8, 2009
_______________________
Correspondence address:
Dr. Fernando Korkes
Rua Pirapora, 167
São Paulo, SP, 04008-060, Brazil
Fax: + 55 11 3884-2233
E-mail: fkorkes@terra.com.br
EDITORIAL COMMENT
Ureteroscopy
is the first line treatment for ureteral lithiasis except in some cases.
Perez-Castro et al. described the technique of lowering the contralateral
limbs to facilitate the expansion and advancement of the ureteroscope
(1). Currently, most of the groups perform the procedure by telesurgery
in the classic lithotomy position, although the position has been modified
to improve access and to facilitate the extraction and removal of stone
fragments. In this article, the authors analyzed the results of ureteroscopy
in two positions; classic lithotomy and lithotomy with homolateral leg
extended, referenced by other authors (2), and they have observed significant
differences in surgical time in men (not in women), without significant
differences in the other parameters analyzed. Endourology techniques have
been performed in different positions to improve the access to the ureter.
Angus et al. reported that increasing the degree of the lithotomy position
improves the access to the iliac ureter (3). On the other hand, Bercowsky
et al. studied infundibulo-pelvic angle of lower calyx and they found
that the lower pole infundibulo-pelvic angle broadens when the patient
lies in a prone 20-degree head down position (4). Herrell et al. used
flank position in ureteroscopy to treat complex calyceal lithiasis because
the extraction is facilitated due to gravity (5).
The results published in this article by
Korkes et al. show that lithotomy with homolateral extended leg position
is a valid approach for ureteral lithiasis and it provides an alternative
to classic lithotomy position. However, it is important to gain more experience
in the use of this position and we must consider studying other parameters
that could influence the results and surgical time, like the size of prostate
gland that in some occasions can render the access and the mobility of
the semi-rigid ureteroscope difficult.
REFERENCES
- Pérez-Castro E, Martínez Piñeiro JA: La ureterorrenoscopia transuretral: un actual proceder urológico. Arch Esp Urol. 1980; 33: 445-60.
- Arrabal Martín M, Ocete Martín C, Jiménez Pacheco A, Miján Ortiz JL, Pareja Vilches M, Zuluaga Gómez A: Metodología y límites de la ureteroscopia ambulatoria Arch Esp Urol. 2006; 59: 261-72.
- Angus DG, Webb DR: Influence of hip flexion on the course of the ureter. Ureteroscopic implications. Eur Urol. 1988; 14: 287-90.
- Bercowsky E, Shalhav AL, Elbahnasy AM, Owens E, Clayman RV: The effect of patient position on intrarenal anatomy. J Endourol. 1999; 13: 257-60.
- Herrell SD, Buchanan MG: Flank position ureterorenoscopy: new positional approach to aid in retrograde caliceal stone treatment. J Endourol. 2002; 16: 15-8.
Dr.
Miguel A. Arrabal-Polo
Section of Urology
San Cecilio University Hospital
Granada, Spain
E-mail: arrabalp@ono.com
EDITORIAL COMMENT
Surgeons have historically been particular about patients’ position
during surgery. This is important for access, minimizing pressure points
and prevention of deep vein thrombosis during extended operation time.
Early experience with the rigid ureteroscopy has identified two regions
of the ureter that can be difficult to negotiate, the first at the vesico-ureteric
junction and the second anterior to the iliac bifurcation. During initial
days of ureteroscopy use of large size (13F or plus) ureteroscopes mandated
that all possible efforts should be made to ease passage of the scope
through narrow parts of the ureter. However, there is dearth of scientific
literature on the efficacy of such maneuvers. Korkes and colleagues (1)
have looked into the impact of the outcome on one position (dorsal lithotomy
with leg extended) over traditional dorsal lithotomy. Although they did
not observe any significant advantage of one procedure over the other,
they have noted some advantage in operative time using extended leg position.
More than two decades ago, Angus and Webb (2) noted that the lower ureter
possesses two curves, an upper curve at the iliac bifurcation that straightens
with increasing degrees of lithotomy and a lower vesical curve in the
pelvis, which is unaltered by patient position. Dagnone et al. (3) applied
lower-abdominal pressure to see if it facilitates semi rigid-ureteroscopy
to access to the upper ureter for safe laser lithotripsy using a 7.5F
scope. They observed that lower-abdominal pressure could be helpful to
negotiate passage of the endoscope over the iliac vessels or to place
the laser fiber on stones.
In conclusion, this is a small basic study
looking at an innocuous modification that may have beneficial impact on
the ease of accessing two difficult points in the distal and middle ureter.
In a larger cohort of patients preferably at a multi institutional setting,
future investigators may be able to note a significant difference.
REFERENCES
- Korkes F, Neto ACL, Mattos MH, Pompeo AC, Wroclawski ER: Patient position and semi-rigid ureteroscopy outcomes. Int Braz J Urol. 2009 [In Press]
- Angus DG, Webb DR: Influence of hip flexion on the course of the ureter. Ureteroscopic implications. Eur Urol. 1988; 14: 287-90.
- Dagnone AJ, Blew BD, Pace KT, Honey RJ: Semirigid ureteroscopy of the proximal ureter can be aided by external lower-abdominal pressure. J Endourol. 2005; 19: 342-7.
Dr.
M. Hammad Ather
Associate Professor
Director Urology Residency Program
Aga Khan University
Karachi, Pakistan
E-mail: hammad.ather@aku.edu
EDITORIAL COMMENT
Ureterorenoscopy
(URS), extracorporeal shock wave lithotripsy (SWL) and percutaneous nephrolithotomy
(PCNL) are the main modalities for modern stone treatment. While all of
these procedures have shown to be as effective minimally invasive treatment
for various stone situations, there are always demands to further excel
their performance. One of the most common ways to improve this situation
is by the help of technological advancement. The development of digital
optics, scope design and auxiliary instruments has greatly improved the
performance of URS and PCNL, in particular flexible instruments (1). Similarly,
there have also been improvements in technology of SWL that can bring
the performance back to the standard set by HM3 (2). However, all these
new developments will inevitably increase the capital cost of medical
treatment, which will be particular important in the current economic
turmoil. As a result, the real impact of these technical advancements
may not be as great as could be expected, especially for the developing
countries.
However, there is also another approach to improve the performance by
modifying the working condition or treatment protocols of the existing
equipment. As well demonstrated by this article, the simple modification
of the leg position will help to improve the performance of semi-rigid
URS (3). This simple and easy approach required no extra-cost for equipment,
but can shorten the operating time, in particular for male patients by
30%. There are also other approaches that have been reported to improve
the performance of URS, such as instillation of lidocaine jelly proximal
to the stone to minimize stone flush back and improve stone free rate
(4). Similarly, modifications of treatment protocols for SWL, such as
modification of shockwave delivery rate (5) and application of gel on
the treatment head (6), has also shown to be effective in the improvement
of treatment outcomes. These kinds of non-costly procedures for improvement
of treatment performance will definitely benefit more patients worldwide
than the simple pursuit of high technological equipment.
One of the pitfalls of this study, as already
discussed by the authors, is the “non-blinded” nature of the
study. As the surgeon performed the operation will know the positioning
of the legs, therefore any subjective preference or bias to one of the
positions may lead to bias in part of the results, such as the operating
time. However, this kind of bias will be intrinsic to most of the surgical
studies and is difficult, if not impossible, to completely eliminate.
Therefore, one should be aware of this bias during the interpretation
of results. Nevertheless, the authors have convincingly demonstrated the
superiority of the dorsal lithotomy position with same side leg slightly
extended (DLEL) over dorsal lithotomy position (DL) during URS. This approach
should be encouraged in our daily practice.
REFERENCES
- Canes D, Desai MM: New technology in the treatment of nephrolithiasis. Curr Opin Urol. 2008; 18: 235-40.
- Nomikos MS, Sowter SJ, Tolley DA: Outcomes using a fourth-generation lithotripter: a new benchmark for comparison? BJU Int. 2007; 100: 1356-60.
- Korkes F, Neto ACL, Mattos MH, Pompeo AC, Wroclawski ER: Patient position and semi-rigid ureteroscopy outcomes. Int Braz J Urol. 2009 [In Press]
- Zehri AA, Ather MH, Siddiqui KM, Sulaiman MN: A randomized clinical trial of lidocaine jelly for prevention of inadvertent retrograde stone migration during pneumatic lithotripsy of ureteral stone. J Urol. 2008; 180: 966-8.
- Semins MJ, Trock BJ, Matlaga BR: The effect of shock wave rate on the outcome of shock wave lithotripsy: a meta-analysis. J Urol. 2008; 179: 194-7; discussion 197.
- Neucks JS, Pishchalnikov YA, Zancanaro AJ, VonDerHaar JN, Williams JC Jr, McAteer JA: Improved acoustic coupling for shock wave lithotripsy. Urol Res. 2008; 36: 61-6.
Dr.
Anthony NG Chi-fai
Associate Professor
Division of Urology
Department of Surgery
The Chinese University of Hong Kong
E-mail: ngcf@surgery.cuhk.edu.hk