ASSESSMENT
OF SERUM CATECHOLAMINE CONCENTRATIONS IN PATIENTS WITH PHEOCHROMOCYTOMA
UNDERGOING VIDEOLAPAROSCOPIC ADRENALECTOMY
(
Download pdf )
MARCOS F. ROCHA, PATRICK TAUZIN-FIN, PAULO L. VASCONCELOS, PHILIPPE BALLANGER
Department of Urology, Hospital Pellegrin-Tondu, Pellegrin University Hospital Center, Bordeaux, France
ABSTRACT
Introduction:
We analyzed the changes in serum catecholamine concentrations, i.e. adrenaline
and noradrenaline, in response to surgical stress in patients with pheochromocytoma
who undergone videolaparoscopic adrenalectomy.
Materials and Methods: Between January 1998
and March 2002, 11 patients underwent 12 videolaparoscopic adrenalectomies.
In one case, the adrenalectomy was bilateral. Serum catecholamines were
measured at 6 surgical times: T0: control before induction; T1: following
the induction, laryngoscopy and intubation sequence; T2: after installing
the pneumoperitoneum; T3: during manipulation-exeresis of the pheochromocytoma;
T4: following ablation of the pheochromocytoma; T5: in the recovery room
following intervention when the patient was extubated and was hemodynamically
stable.
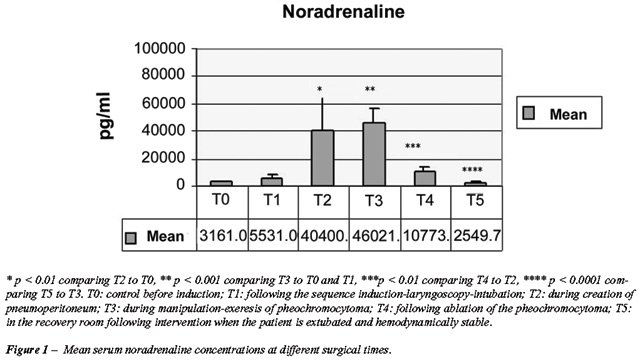
Results: Mean concentrations of serum noradrenaline
were significantly different when the T0 and T2 surgical times were compared
(T0: 3161 pg/mL; T2: 40440 pg/mL; p < 0.01), T0 and T3 (T0: 3161 pg/mL;
T3: 46021 pg/mL; p < 0.001), T1 and T3 (T1: 5531 pg/mL; T3: 46021 pg/mL;
p < 0.01), T2 and T4 (T2: 40440 pg/mL; T4: 10773 pg/mL; p < 0.01)
and T3 and T5 (T3: 46021 pg/mL; T5: 2549 pg/mL; p < 0.001). Mean concentrations
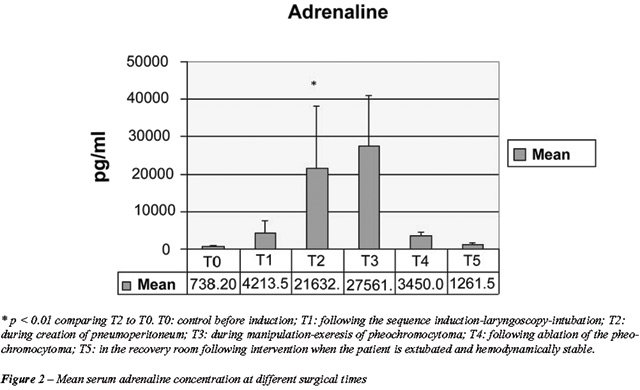
of serum adrenaline were significantly different when the T0 and T3 surgical
times were compared (T0: 738 pg/mL; T3: 27561 pg/mL; p < 0.01).
Conclusion: The pneumoperitoneum significantly
increases serum noradrenaline concentrations, manipulation of the adrenal
gland significantly increases the serum concentrations of noradrenaline
and adrenaline, and the pheochromocytoma ablation significantly decreases
serum noradrenaline concentrations.
Key
words: pheochromocytoma; laparoscopy; catecholamines
Int Braz J Urol. 2005; 31: 299-308
INTRODUCTION
Pheochromocytoma
is an uncommon and important neoplasia because, despite its rarity, it
is associated with catecholamine-induced hypertension, which can be resolved
by neoplasia excision. The definitive treatment for pheochromocytoma is
surgical ablation of the adrenal gland and/or paragangliomas. Before the
1950s, the peroperative mortality was between 20 and 25% of cases with
a preoperative diagnosis of pheochromocytoma and around 50% of cases without
a preoperative diagnosis of pheochromocytoma. The lack of proper control
for hypertensive crises and cardiac arrhythmias during manipulation and
ablation of the pheochromocytoma was responsible for this high mortality.
The advances in peroperative control and the preoperative introduction
of alpha 1-adrenergic blockade have significantly reduced mortality rates
(1).
The first laparoscopic adrenalectomies were
described by Gagner et al. and Higashihara et al. in 1992 (2,3). Studies
have shown that videolaparoscopic adrenalectomy offers lower morbidity
than open surgery (4,5). The videolaparoscopic technique has become the
preferred option for treating adrenal tumors (6), however some doubts
remain about the use of videolaparoscopy for management of pheochromocytomas
due to cardiovascular risks that are potentially higher when compared
to open surgery. Such risks are related to catecholamine release. Factors
such as the use of carbon dioxide, the increase in abdominal tension and
manipulation of the adrenal gland have been implied in catecholamine release
(7).
Thus, in order to validate the videolaparoscopic
technique in the management of pheochromocytomas, it is important to determine
potential changes in serum catecholamine concentrations, as well as the
relationship between such changes and higher cardiovascular risk.
This study aimed to assess changes in serum
catecholamine concentrations, i.e. adrenaline and noradrenaline, in response
to surgical stress in patients with pheochromocytoma undergoing videolaparoscopic
adrenalectomy.
MATERIALS AND METHODS
The
study was performed between January 1998 and March 2002 in 11 patients
undergoing 12 videolaparoscopic adrenalectomies. The study included patients
diagnosed with pheochromocytoma, which was confirmed through dosing of
serum and urinary catecholamines. Abdominal and pelvic computerized tomography
was performed in 8 patients, magnetic resonance imaging in 10 patients
and scintigraphy with 131I-metaiodobenzylguanidine in 10 patients.
Blood collections for dosing catecholamines,
adrenaline and noradrenaline, by high-pressure liquid chromatography (HPLC)
were performed at the following times: T0: control before induction; T1:
following the induction, laryngoscopy and intubation sequence; T2: during
the creation of pneumoperitoneum; T3: during manipulation-extraction of
the pheochromocytoma; T4: following ablation of the pheochromocytoma;
T5: in the recovery room following the intervention when the patient was
extubated and hemodynamically stable.
All patients underwent preoperative cardiovascular
assessments, including Doppler echocardiography and 24-hour Holter. Preparation
started 15 days before the intervention by associating a alpha 1 blocker
(prazosin: alpress® LP 5 mg/day) and a beta 1 blocker (bisoprolol:
détensil® 10 to 20 mg/day). Three days before the intervention,
an intravenous alpha 1 blocker, urapidil® (250 mg/day in continuous
perfusion and hourly control of blood pressure), was started as a replacement
to oral therapy and maintained until the end of the intervention. Oral
pre-anesthetic medication consisted of 5 mg midazolam (short-acting benzodiazepine)
associated with 0.5 mg atropine (muscarinic receptor blocker).
General anesthesia was standardized as follows:
induction with propofol (2-2.5 mg/Kg-1) and sufentanil (0.8-1
µg/Kg-1) IV for control of blood pressure (BP), orotracheal
intubation facilitated by cisatracurium 0.15 mg.Kg-1; maintenance
with continuous perfusion of sufentanil and cisatracurium and administration
of sevoflurane or isoflurane with pure oxygen. Following induction, BP
was continuously monitored using an arterial catheter connected to a blood
pressure meter (Baxtertm). Hydration was started with crystalloids
10-15 mL/Kg-1/h-1 (isotonic saline solution, Ringer
solution). Ventilation was adapted in order to maintain the PCO2
between 35 and 45 mmHg. Urapidil was maintained in a continuous infusion
of 10 mg/h-1 until ligation of the adrenal vein. Tension peaks
were defined as systolic blood pressure (SBP) over 160 mmHg, and were
treated through administering nicardipine (2-4 mg) aiming to maintain
SBP between 120-160 mmHg. Episodes of sinus tachycardia, as defined by
a heart rate (HR) over 100-120 b/min-1, were treated by the
administration of esmolol 100 mg in order to maintain the HR under 100
b/min-1. Cardiovascular shock, as defined by SBP lower than
80 mmHg, was treated by administering ephedrine 3-6 mg IV.
The adrenalectomies were performed as described
by Rocha et al., 2003 (8). Patients were positioned in lateral decubitus
opposite the lesion. Four trocars were used - 3 10-mm and one 5-mm. The
first trocar (10 mm) was introduced by “open” laparoscopy
to the lateral margin of the rectus muscle of the abdomen approximately
4 cm cranial to the umbilical scar. The second trocar (10 mm) was placed
on the epigastric midline. The third trocar (10 mm) was placed lateral
to the first trocar, between the lateral margin of the rectus muscle of
the abdomen and the anterior axillary line. The fourth trocar (5 mm) was
placed lateral to the third trocar, between the anterior axillary line
and the middle axillary line. The pneumoperitoneum was maintained at 12
mmHg. When the left adrenal gland was operated on, the intra-abdominal
procedure started with an incision in the parietocolic gutter and dissection
of two thirds of the descending colon. The spleen was withdrawn to expose
the upper region of the renal cavity. The left renal vein was dissected
and the adrenal vein was then identified, dissected and sectioned with
metallic clips. Following this, the adrenal gland was dissected on the
cleavage plane between the adrenal gland and the kidney. Arteries and
occasional small accessory veins were sectioned with clips or after bipolar
coagulation around the gland. The adrenalectomy specimen was removed inside
an endosac (Endocath 10®) through a trocar orifice that was enlarged
by 1 cm on each side. The trocar orifices were closed in 2 planes. When
the right adrenal gland was operated on, the right liver lobe was withdrawn
after sectioning of the triangular ligament. The renal cavity was exposed
above the right colic angle. The cava vein was dissected up to the adrenal
vein, which was then sectioned with clips. The following surgical times
were similar to the left adrenalectomy.
The ligation of the adrenal vein was performed
early, with minimal previous dissection of the adrenal gland.
To statistically analyze the results, Graphpad
Prism software was employed, using non-parametric methods: Kruskal-Wallis
test and Dunn’s multiple comparisons test.
The statistical significance value was established
at 95 % (p < 0.05).
RESULTS
No
surgical conversion was required. The mean length of intervention was
127 min (75 to 195 min). Blood loss was between 0 and 1000 mL with a mean
value of 105 mL.
The mean serum noradrenaline concentrations
were significantly different (p < 0.05) when comparing T0 and T2 surgical
times (T0: 3161 pg/mL; T2: 40440 pg/mL; p < 0.01), T0 and T3 (T0: 3161
pg/mL; T3: 46021 pg/mL; p < 0.001), T1 and T3 (T1: 5531 pg/mL; T3:
46021 pg/mL; p < 0.001), T2 and T4 (T2: 40440 pg/mL; T4: 10773; p <
0.01) and T3 and T5 (T3: 46021 pg/mL; T5: 2549 pg/mL; p < 0.001). There
was no statistical difference (p > 0.05) when the other surgical times
were compared (Figure-1).
Mean serum adrenaline concentrations were
significantly different when comparing the T0 and T3 surgical times (T0:
738 pg/mL; T3: 27561 pg/mL; p < 0.01). There was no statistical difference
(p > 0.05) when the other surgical times were compared (Figure-2).
During the creation of the pneumoperitoneum
(T2), 6 hypertension peaks were observed, which were associated with sinus
tachycardia in 3 cases. Manipulation or exeresis of the adrenal gland
(T3) caused 8 hypertension peaks associated with sinus tachycardia in
2 cases.
Patient 5 presented atrial and ventricular
extrasystoles during these 2 surgical times (T2 and T3) and was treated
with intravenous (IV) esmolol.
The therapeutic outcome was reached in all
cases, with SBP decreasing from 178 +/- 12 to 129 +/- 11 mmHg (p <
0.001) and diastolic blood pressure (DBP) from 99 +/- 13 to 73 +/- 11
mmHg (p < 0.001).
Following tumor ablation (T4), 5 hypertensive
episodes were observed (Table-1).
Return to oral diet occurred between the
first (D1) and the third (D3), with a mean of 1.9 days. Removal of the
drain occurred between D2 and D3. Deambulation was authorized between
D1 and D3 with a mean of 2.18 days. Discharge from hospital occurred between
D3 and D6 with a mean hospital stay of 3.8 days. There was one damage
to the adrenal vein, which was treated during surgery with no need for
conversion to open surgery. This patient received transfusion of 2 units
of red blood cells concentrate.
All patients were reassessed 6 months after
intervention and presented normalized BP with no requirement for treatment.
COMMENTS
Laparoscopy
effectively offers advantages for open surgery, that is less severe postoperative
pain, early deambulation, reduced hospital stay and prompter return to
daily activities (9,5). However, the surgery for management of pheochromocytoma
differs from the approach used for other adrenal tumors due to the increased
cardiovascular risks during the surgical intervention related to catecholamine
release (2,10).
This study confirms that creation of pneumoperitoneum
and tumor manipulation during videolaparoscopic ablation of pheochromocytoma
are accompanied by a significant release of serum catecholamines. This
release is probably responsible for hemodynamic disorders such as hypertensive
peaks and sinus tachycardia.
Insufflation of pneumoperitoneum is associated
with an increase in serum catecholamines, either by stimulus to mechanical
compression or a change in tumor vascularization (11,12). Additionally,
carbon dioxide used to insufflate the pneumoperitoneum can lead to hypercapnia,
which would increase sympathetic tonus, thus changing tension levels (13).
In the cases evaluated in this study, the
creation of the pneumoperitoneum produced an important release of noradrenaline
into the blood stream, thus increasing its concentration when compared
with preoperative values (p < 0.01). This release was variable and
unpredictable between one patient and the other. In this series, pneumoperitoneum
increased mean serum noradrenaline concentrations 12.7 times the baseline
value and mean serum adrenaline concentrations increased 29.3 times the
baseline value. These results are in agreement with the study by Joris
et al. (7), who observed an increase in plasma catecholamine concentrations
by 7 to 16 times the baseline value following the creation of pneumoperitoneum
in patients with pheochromocytoma undergoing videolaparoscopic surgery.
Manipulation and ablation of the pheochromocytoma
during laparoscopy equally produce an exaggerated release of serum catecholamines
(14). In the series described in this study, manipulation and exeresis
of pheochromocytoma (T3) evolved with high concentrations of serum noradrenaline
and adrenaline. When assessing the mean concentrations of serum noradrenaline
(p < 0.001) and adrenaline (p < 0.01), statistical differences were
observed between T3 and pre-induction control (T0). In this series, despite
early ligation of the adrenal vein, we observed an elevation in catecholamine
concentrations during dissection of the adrenal gland.
According to some authors, tension variations
are less important or equivalent during laparoscopy when compared to laparotomy
(11). Joris et al. (15), studied hemodynamic changes relative to pneumoperitoneum
with carbon dioxide in 20 healthy patients undergoing elective laparoscopic
cholecystectomy. They also assessed the changes in several neurohumoral
mediators, which can contribute to hemodynamic changes, such as plasma
concentrations of cortisol, catecholamines, vasopressin, renin, endothelin
and prostaglandins. Peritoneal insufflation resulted in significant reduction
in cardiac output, as well as an increase in blood pressure and systemic
and pulmonary vascular resistance. Laparoscopy resulted in a progressive
and significant increase in plasma concentrations of cortisol, adrenaline,
noradrenaline, renin and vasopressin. Prostaglandins and endothelins showed
no significant change. The authors concluded that vasopressin and catecholamines
probably measured the increase in systemic vascular resistance during
insufflation of pneumoperitoneum with carbon dioxide.
Fernandez-Cruz et al. (10), reported that,
in the case of pheochromocytomas, videolaparoscopic adrenalectomy is associated
with a lesser increase in catecholamine levels in peripheral circulation
when compared with laparotomy, and that hypertensive peaks are related
to direct manipulation of the adrenal gland. The authors compared 23 videolaparoscopic
adrenalectomies (non-functioning adenomas, aldosterone-producing adenoma,
Cushing’s adenoma and Cushing’s disease) using insufflation
of pneumoperitoneum with carbon dioxide, with 8 videolaparoscopic adrenalectomies
for pheochromocytoma using insufflation of pneumoperitoneum with helium,
and with eight 8 adrenalectomies performed by the conventional open approach.
They studied the serum changes in catecholamine levels and correlated
them with intraoperative cardiovascular disorders in patients with pheochromocytoma.
There was no significant difference between videolaparoscopic adrenalectomies
due to pheochromocytoma compared to videolaparoscopic adrenalectomies
due to other lesions, as regards surgical time, blood loss, hospital stay
and return to usual activities. Results for these parameters were unfavorable
to the open adrenalectomies group. A major increase in plasma catecholamine
levels occurred in patients with pheochromocytoma during tumor manipulation
in the videolaparoscopy group (17.4 times for adrenaline and 8.6 times
for epinephrine) and in the open surgery group (34.2 times for adrenaline
and 13.7 for noradrenaline). Cardiovascular instability was associated
with open surgery only.
Among the studied cases, in 6 out of 12
adrenalectomies (50%), hypertensive peaks occurred during the creation
of pneumoperitoneum (T2) and in 8 out of 12 adrenalectomies (66.6%), hypertensive
peaks occurred during manipulation and exeresis of the gland. These hemodynamic
changes occurred simultaneously with an increase in catecholamine levels
during the creation of pneumoperitoneum and manipulation / exeresis of
the gland.
Two independent predictive factors for perioperative
morbidity are the secreting characteristic of the tumor, and its size
(16). An excessive and unpredictable peroperative catecholamine release
can lead to a serious clinic condition associated with malignant hypertension,
mydriasis, pulmonary edema (17) and even acute heart failure (18).
Despite the association between the creation
of pneumoperitoneum (T2) and manipulation (T3) of the adrenal gland with
an increase in serum rates of noradrenaline and adrenaline, the adrenalectomies
were performed with low morbidity. A laparoscopic exeresis of pheochromocytoma
can be performed, but it requires proper preoperative preparation and
careful perioperative anesthetic surveillance of blood pressure and occasional
cardiac arrhythmias. The preoperative preparation is intended to decrease
cardiovascular morbidity and includes alpha adrenergic blockade and, if
required, beta adrenergic blockade. Hypertensive peaks in pheochromocytoma
are related to the stimulation of alpha 1 receptors (19). In the series
under study, preoperative control was achieved by previous blockade of
alpha 1 receptors by prazosin and urapidil. Beta adrenergic blockade is
not systematic and depends on the presence of associated tachycardia (19).
Two problems occur during pheochromocytoma
surgery, and they require opposite solutions: 1) the catecholamine release
during tumor manipulation leads to a risk of paroxysmal hypertension and
episodes of sinus tachycardia, which can be effectively treated by associating
nicardipine (calcium channel antagonist) and esmolol (selective beta blocker);
2) the significant decrease in catecholamine levels following tumor ablation
can, contrarily, cause severe hypotension, which can be worsened by the
persistent effects of alpha 1-antagonist drugs that have been introduced
during preoperative preparation (19). Thus, the use of alpha 1-antagonists
(Urapidil®) available for injection with short half-live and short
action can be used during the preoperative period, offering a potential
solution to both problems (20).
In a series with 8 patients, Joris et al.
(7) used alpha 1-adrenergic blockers for preoperative preparation. During
the intervention, they used an infusion of nicardipine (calcium channel
blocker) for treating and preventing increases in blood pressure. Six
of the 8 patients (75%) showed increased blood pressure higher than 25%
of the baseline value during the creation of pneumoperitoneum. The authors
reported that hemodynamic changes were easily treated through a continuous
infusion of nicardipine associated with a beta blocker. The authors stated
that no episode of acute hypotension (blood pressure lower than 60 mmHg)
was observed in the 8 patients, probably because they had received vasodilators
and/or were normotensive before surgery.
In the present series, during 12 adrenalectomies,
5 of the patients (41.6%) had hypotensive episodes and systolic blood
pressure lower than 80 mmHg, and were treated by administering bolus ephedrine
and volume reposition with crystalloids. However, no patient in this series
presented pressure levels under 60 mmHg. Episodes of hypotension were
related to the decrease in serum catecholamine concentrations observed
after ablation of the gland. Serum noradrenaline concentrations, following
adrenal ablation (T4), significantly decreased (p < 0.01) when compared
with serum noradrenaline levels during creation of pneumoperitoneum (T2).
When compared at T4 and T2, the decrease in serum adrenaline concentrations
was not significant, probably due to the reduced number of study cases
and the large variation in serum adrenaline concentration among the patients.
This study is in agreement with data from
the literature, showing that videolaparoscopic adrenalectomy is feasible
for management of pheochromocytomas and presents a low morbidity rate.
The creation of pneumoperitoneum and the manipulation of the adrenal gland
are related to an increase in serum catecholamines concentrations, and
the ablation of the pheochromocytoma is related to a decrease in noradrenaline
concentrations. In some cases, the changes in serum catecholamine concentrations
correlate with hemodynamic disturbances, which, however, were easily treated.
CONCLUSION
The barotrauma promoted by installing the pneumoperitoneum with a pressure of 12 mmHg in patients with pheochromocytoma induced a significant increased in serum noradrenaline concentrations. In patients with pheochromocytoma undergoing videolaparoscopic adrenalectomy, surgical stress during manipulation of the adrenal gland promoted significant increases in serum concentrations of noradrenaline and adrenaline. The serum noradrenaline concentrations significantly decreased following ablation of the pheochromocytoma when compared with serum concentrations during creation of pneumoperitoneum and manipulation of adrenal gland.
REFERENCES
- Lucon AM, Latronico AC: Malignant and Benign Supra-renal Diseases. In: Barata HS, Carvalhal GF (eds.), Urology Principles and Practice. Porto Alegre, ArtMed. 1999; pp. 581-90. [in Portuguese]
- Gagner M, Lacroix A, Bolte E: Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med. 1992; 14: 1033.
- Higashihara E, Tanaka Y, Horie S, Aruga S, Nutahara K, Homma Y, el al.: A case report of laparoscopic adrenalectomy. Nippon Hinyokika Gakkai Zasshi. 1992; 83: 1130-3.
- Bonjer HJ, Sorm V, Berends FJ, Kazemier G, Steyerberg EW, De Herder WW, et al.: Endoscopic retroperitoneal adrenalectomy: lessons learned from 111 consecutive cases. Ann Surg. 2000; 232: 796-803.
- Winfield HN, Hamilton BD, Bravo EL, Novick AC: Laparoscopic adrenalectomy: the preferred choice? A comparison to open adrenalectomy. J Urol. 1998; 160: 325-9.
- Suzuki K, Kageyama S, Hirano Y, Ushiyama T, Rajamahanty S, Fujita K: Comparison of 3 surgical approaches to laparoscopic adrenalectomy: a nonrandomized, background matched analysis. J Urol. 2001; 166: 437-43.
- Joris JL, Hamoir EE, Hartstein GM, Meurisse MR, Hubert BM, Charlier CJ, et al.: Hemodynamic changes and catecholamine release during laparoscopic adrenalectomy for pheochromocytoma. Anesth Analg. 1999. 88: 16-21.
- Flavio Rocha M, Faramarzi-Roques R, Tauzin-Fin P, Vallee V, Leitao de Vasconcelos PR, Ballanger P: Laparoscopic surgery for pheochromocytoma. Eur Urol. 2004; 45: 226-32.
- Castilho LN: Suprarrenalectomy. In: Castilho LN (ed.), Urologic Laparoscopy. Campinas, LPC comunicações. 2000. pp. 365-378. [in Portuguese]
- Fernandez-Cruz L, Taura P, Saenz A, Benarroch G, Sabater L: Laparoscopic approach to pheochromocytoma: hemodynamic changes and catecholamine secretion. World J Surg. 1996. 20: 762-8; discussion 768.
- de La Chapelle A, Deghmani M, Dureuil B: Peritoneal insufflation can be a critical moment in the laparoscopic surgery of pheochromocytoma. Ann Fr Anesth Reanim. 1998; 17: 1184-5.
- Mann C, Millat B, Boccara G, Atger J, Colson P: Tolerance of laparoscopy for resection of phaeochromocytoma. Br J Anaesth. 1996; 77: 795-7.
- Fernandez-Cruz L, Saenz A, Taura P, Benarroch G, Nies C, Astudillo E: Pheochromocytoma: laparoscopic approach with CO2 and helium pneumoperitoneum. Endosc Surg Allied Technol. 1994; 2: 300-4.
- Meurisse M, Joris J, Hamoir E, Hubert B, Charlier C: Laparoscopic removal of pheochromocytoma. Why? When? and Who? (reflections on one case report). Surg Endosc. 1995; 9: 431-6.
- Joris JL, Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML: Hemodynamic changes induced by laparoscopy and their endocrine correlates: effects of clonidine. J Am Coll Cardol. 1998; 32: 1389-96.
- Kinney MA, Warner ME, van Heerden JA, Horlocker TT, Young WF Jr., Schroeder DR, et al.: Perianesthetic risks and outcomes of pheochromocytoma and paraganglioma resection. Anesth Analg. 2000; 91: 1118-23.
- Tauzin-Fin P, Hilbert G, Krol-Houdek M, Gosse P, Maurette P: Mydriasis and acute pulmonary oedema complicating laparoscopic removal of phaechromocytoma. Anaesth Intensive Care. 1999; 27: 646-9.
- Quezado ZN, Keiser HR, Parker MM: Reversible myocardial depression after massive catecholamine release from a pheochromocytoma. Crit Care Med. 1992; 20: 549-51.
- Colson P, Ribstein J: Simplified strategy for anesthesia of pheochromocytoma. Ann Fr Anesth Reanim. 1991; 10: 456-62.
- Valat P, Gosse P, Roche A: Urapidil during surgery of pheochromocytoma: should begin in the pre-operative period. Ann Fr Anesth Reanim. 1996; 15: 698-9.
_______________________
Received: February 2, 2005
Accepted after revision: June 10, 2005
_______________________
Correspondence
address:
Dr. Marcos Flávio Rocha
Rua Israel Bezerra, 1040 / 902
Fortaleza, CE, Brazil
Fax: + 55 85 3477-4440
E-mail: marcosflaviohr@yahoo.com.br
EDITORIAL COMMENT
The
authors are to be congratulated for their excellent paper on laparoscopic
surgery for pheochromocytoma but, in fact, the authors’ overall
conclusions were already expected.
Many
papers concur that during adrenal manipulation (either laparoscopic or
open), an increase in serum catecholamine usually occurs, with the possibility
of hemodynamic events (1-5). As well, other papers have already shown
the effects of pneumoperitoneum on the intra-abdominal vasculature - namely
an increase in vascular resistance, a decrease in venous drainage and
consequently, transient renal and liver dysfunction, intestinal congestion
and increased serum catecholamine release. After desufflation, all parameters
return to normal levels (6-10).
Unfortunately,
there was no open adrenalectomy control group in order to compare the
results.
REFERENCES
1. Kinney MA, Warner
ME, van Heerden JA, Horlocker TT, Young WF Jr., Schroeder DR, et al.:
Perianesthetic risks and outcomes of pheochromocytoma and paraganglioma
resection. Anesth Analg. 2000; 91: 1118-23.
2. Turner MC, Lieberman E, DeQuattro V: The peri-operative management
of pheochromocytoma in children. Clin Pediatr (Phila). 1992; 31: 583-9.
3. Marty J, Desmonts JM, Chalaux G, Fischler M, Michon F, Mazze RI, et
al.: Hypertensive responses during operation for phaeochromocytoma: a
study of plasma catecholamine and haemodynamic changes. Eur J Anaesthesiol.
1985; 2: 257-64.
4. Kim HH, Kim GH, Sung GT: Laparoscopic adrenalectomy for pheochromocytoma:
comparison with conventional open adrenalectomy. J Endourol. 2004; 18:
251-5.
5. Kazaryan AM, Kuznetsov NS, Shulutko AM, Beltsevich DG, Edwin B: Evaluation
of endoscopic and traditional open approaches to pheochromocytoma. Surg
Endosc. 2004; 18: 937-41.
6. Dunn MD, McDougall EM: Renal physiology. Laparoscopic considerations.
Urol Clin North Am. 2000; 27: 609-14.
7. McDougall EM, Monk TG, Wolf JS Jr, Hicks M, Clayman RV, Gardner S,
et al.: The effect of prolonged pneumoperitoneum on renal function in
an animal model. J Am Coll Surg. 1996; 182: 317-28.
8. Joris JL, Hamoir EE, Hartstein GM, Meurisse MR, Hubert BM, Charlier
CJ, et al.: Hemodynamic changes and catecholamine release during laparoscopic
adrenalectomy for pheochromocytoma. Anesth Analg. 1999; 88: 16-21.
9. Joris JL, Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML: Hemodynamic
changes induced by laparoscopy and their endocrine correlates: effects
of clonidine. J Am Coll Cardiol. 1998; 32: 1389-96.
10. Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML: Hemodynamic
changes during laparoscopic cholecystectomy. Anesth Analg. 1993; 76: 1067-71.
Dr. Tibério M. Siqueira Jr.
Section of Laparoscopic Urology
Getúlio Vargas Hospital
Recife, PE, Brazil